ACHAIKI IATRIKI | 2023; 42(4):179–189
Review
Sofia Krontira*, Petros Mantzios*, Konstantinos Thomopoulos, Christos Konstantakis
Department of Internal Medicine, Division of Gastroenterology, University of Patras Medical School, Patras, Greece
*Equally contributing first authors
Received: 14 Apr 2023; Accepted: 05 Sep 2023
Corresponding author: Christos Konstantakis, MD PhD, Consultant Gastroenterologist, University Hospital of Patras, 26504 Patras, Greece, E-mail: asraiah@yahoo.com
Key words: Paediatric dysphagia, assessment, management, speech and language pathologist
Abstract
Ingestion of foreign bodies or caustic substances constitutes an emergent diagnostic and therapeutic challenge, with potentially high morbidity and mortality. Identification of the ingested agent and determination of intention are of paramount importance, as they dictate the appropriate treatment and forecast the overall outcome. Both situations require high levels of suspicion by the treating physician, early recognition and implementation of emergency treatment protocols in order to optimize patient outcomes. A multidisciplinary approach is often required.
INTRODUCTION
Injuries of the upper GI (gastrointestinal tract) include, among others, the ingestion of foreign bodies and corrosive agents. Although relatively uncommon, these conditions are associated with potentially high morbidity and mortality.
The ingestion of foreign bodies is confronted in everyday clinical practice, particularly in paediatric patients [1,2]. In the adult population, on which this current review aims to focus, ingestion is usually associated with accidental food bolus impaction, sometimes in the presence of underlying anatomical abnormalities or motility disorders [3]. While the vast majority of ingested objects cross the gastrointestinal tract without complications, endoscopic intervention may be required in up to 20% of cases [4-6]. Treatment selection depends both on the location of impaction and characteristics of the foreign body, including size, shape and material [7].
The ingestion of corrosive chemicals still represents a major issue in developed countries, despite the implementation of educational programs and preventive measures by western governments [8-10]. In developing countries, its occurrence is still increasing [11-13]. Epidemiological data are scarce and the phaenomenon is widely underreported. Therefore, management of these cases remains a challenge [14]. In adults, the consumption of corrosive agents is usually intentional and associated with extensive damage and long-term complications. On the contrary, children tend to ingest caustic chemicals with exploratory intention and present with mild injuries.
This review aims to outline the evolving data on the epidemiology, diagnostic approach and appropriate management of these conditions, based on updated guidelines published by gastroenterological and endoscopic societies. For the purpose of this manuscript, two separate MEDLINE and PUBMED searches from 1975-2022 were performed to evaluate relevant articles, with priority to high quality publications of the last five years.
FOREIGN BODY INGESTION AND FOOD BOLUS IMPACTION
Epidemiology
Foreign body ingestion constitutes a gastroenterological emergency, accounting for almost 5% of all urgent endoscopies undertaken. More than 100.000 cases per year are reported in the US [2,14,15]. As expected, epidemiological data differ across age groups. In the paediatric population ingestion is more common and almost exclusively accidental/exploratory (98%), with coins being the objects most frequently encountered (66%), followed by toys, magnets and batteries [1,2,16]. On the other hand, food bolus impaction remains the primary cause in adult patients, while true foreign body ingestion is more commonly observed in the presence of psychiatric disorders, impaired mental status, intoxication or for secondary gain in incarcerated patients [3,17]. Edentulous condition and use of prosthetic dentures is another risk factor in elderly patients [3,20].
Gastroenterologists should be aware that food bolus impaction, in 45–75% of cases, occurs in the context of pre-existing oesophageal abnormalities, such as peptic strictures or oesophageal rings [3,4,7]. Achalasia and other motility disorders may also be present. Interestingly, food bolus impaction is rarely a presenting symptom of oesophageal malignancies [3,4]. Eosinophilic oesophagitis is another emerging recognised risk factor (33–40%), characterised by infiltration of the oesophageal mucosa by eosinophils, causing nonspecific symptoms and long term, non-reversible narrowing [3,7]. The diagnosis is confirmed through biopsy. Therefore, current guidelines emphasise the need of histologic evaluation in all patients with suspicious endoscopic findings in order to recognise underlying pathology and prevent symptom recurrence [3,4,6,14].
Initial evaluation
Patient history is the initial and often defining step in the diagnostic approach. Patient symptomatology at first presentation may differ between cases, depending on the type of the foreign body and the degree of obstruction. Usually, there is a clear correlation between time of ingestion and onset of symptoms. For non-communicative patients and children, a reliable history depends on relatives who witnessed the incident. Information on patient comorbidities and the characteristics of the foreign body (size, shape and material) will assist in treatment planning.
Patients may present with acute chest pain and dysphagia or odynophagia, nausea and vomiting. The presence of blood-stained saliva is an alarming feature, suggestive of possible laceration. Retrosternal discomfort is common; however, the area of discomfort is not helpful in determining the exact site of impaction, because of pain radiation [15]. Respiratory distress or wheezing are usually indicative of upper airway obstruction or tracheal compression by oesophageal oedema. Hypersalivation (inability to manage secretions) is suggestive of complete oesophageal obstruction and warrants prompt management. Vital signs, airway status and hemodynamic stability should always be assessed at baseline. Other causes of thoracic pain need to be excluded through biochemical work-up and 12-lead ECG. Areas of anatomic narrowing located above the ligament of Treitz, such as the upper and lower oesophageal sphincter, the aortic notch and the left main stem bronchus are associated with higher impaction risk. After successful food bolus removal some patients experience a persistent subjective feeling mimicking dysphagia for some time (usually up to 24 hours). Patients need to be reassured and followed-up accordingly [3,6].
Clinical signs of oesophageal perforation include fever, edema in the neck and chest area and subcutaneous crepitus. Sharp pointed objects may cause peritonitis by piercing through the GI tract, especially in areas with acute angulation (10). Abdominal guarding, reduced bowel sounds and systemic inflammation symptoms are common in such cases [16]. Surgical intervention is the treatment of choice.
Radiographic evaluation, using biplane radiographs may be helpful in case of ingested radiopaque bodies. Neck, chest and abdomen radiographs can help reveal the exact number and configuration of ingested items and assess for complications by revealing the presence of free air in the mediastinum or under the diaphragm, or lung aspiration. However, their usefulness is limited when concerning radiolucent foreign objects and (non-bony) food bolus content. A classification of commonly encountered items, according to radiodensity, is provided in Table 1.
ESGE and ASGE guidelines propose the use of computed tomography imaging (CT), especially when high index of suspicion for complications exists, in difficult cases (i.e., above the upper oesophageal sphincter / throat – ENT region) [3,18,20]. CT scan, with its superior diagnostic accuracy (70–100%) and ability for 3D reconstruction, provides detailed information on the location and size of foreign bodies and confirms the nature and extent of complications (i.e. abscess, aortoesophageal fistula formation), and therefore is recommended in cases of suspected perforation [3,18-20].
Notably, guidelines recommend strongly against the use of contrast-enhanced radiographic imaging, using oral mediums (barium, gastrografin). These agents compromise direct visualisation by the endoscopist and are associated with risk of pulmonary oedema if aspirated [3,14,18,20].
Conservative management
Each case of ingestion is unique and presents a different challenge. Up to 90% of ingested foreign bodies will cross the GI tract uneventfully, without requiring further intervention [3,20]. As such, a “watch-and-wait” approach should be chosen for asymptomatic ingestion of blunt, short (<5-6 cm length) and narrow (<2.5 cm diameter) objects (batteries and magnets are excluded). ESGE also recommends conservative management in cases of “body packing” (intentional hiding of packaged, illegal narcotic substances in a person’s GI system) in order to avoid accidental leakage and subsequent systemic toxicity. In this way, 95% of parcels will be expelled automatically. Inpatient observation and use of PEG laxatives has been implemented, causing bowel irrigation and facilitating quicker passage. If symptoms of obstruction or toxicity present, or when parcels fail to progress beyond 48 hours, surgical referral is necessary [3,7].
Endoscopic management
In the subset of patients that will not benefit from conservative management, endoscopic treatment is usually undertaken. Flexible endoscopes are considered the primary option, providing excellent diagnostic accuracy (even in the absence of imaging findings) and concurrent management. Oesophagogastroduodenoscopy (EGD) is usually performed under conscious sedation in adults. Endotracheal intubation might be needed in cases of high aspiration risk or poor cooperation, like children, patients with a full stomach or select cases of oesophageal impaction [3,20]. The reported success rate exceeds 95%. ESGE and ASGE guidelines also recommend the use of special equipment, including an overtube or a protective hood, placed over the endoscopic device to prevent mucosal injury during retrieval of sharp objects, while reducing the incidence of aspiration and facilitating foreign body extraction [3,20,21].
The role of rigid endoscopy (RE) in the current ASGE guidelines is complementary to flexible endoscopy (FE). Interestingly, this procedure is not included in the 2016 ESGE guidelines. ENT physicians are accustomed to the use of the rigid oesophagoscopes with excellent results in removal of foreign bodies lodged in the upper oesophagus and hypopharynx, proximally to the upper oesophageal sphincter. Navigation/manipulation of the upper oesophagus with RE appears to be more effective in the hands of experienced users compared with FE. Interestingly, a large meta-analysis conducted by Ferrari et al in 2018 reported no statistically significant difference between RE and FE in terms of foreign object removal success rates and frequency of complications [21].
A wide range of retrieval devices is available and selection depends on the ability and experience of the endoscopist, as well as the size, shape and location of the foreign object. Retrieval forceps of various configurations (alligator forceps being the most commonly used), standard biopsy forceps, retrieval nets (usually indicated for small blunt object or en bloc food bolus removal) and the widely available and economic polypectomy snares have all been used. Endoscopic baskets, such as the Dormia basket, are ideal for removing round and slippery objects. Before intervention, endoscopists are encouraged to rehearse grabbing an object similar to the one ingested, in order to choose the device best suited to the task, thus reducing procedure time and endoscopy related risks [3,6,20].
Food boluses remain the most common foreign bodies in the adult population. The endoscopist usually implements the ”gentle push” technique, using the flexible endoscope to apply pressure on the central part of the bolus and advance it past the gastroesophageal junction and into the stomach. Larger boluses might need to be fragmented before the procedure is completed. Since undiagnosed anatomical disorders are often present, guidelines advise against over exerting pressure blindly especially when met with resistance. In such instances, an attempt to by-pass the bolus, or an en bloc or piecemeal removal is performed, using either a polypectomy snare or a retrieval basket and net [3,20,22]. If eosinophilic oesophagitis is suspected, biopsy specimens should be obtained, even in the presence of a macroscopically normal oesophagus. In the presence of strictures or rings, dilation may be performed concurrently or after a monthly period of proton pump inhibitor administration [3,6]. Figure 1 shows food bolus impacted in the lower oesophagus of a 52-year-old male.
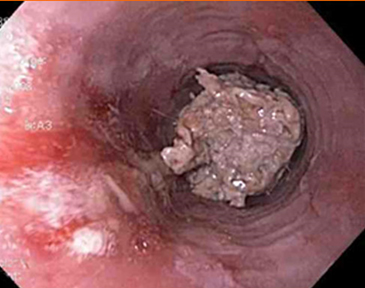
Figure 1. Food bolus impacted in the lower oesophagus of a 52-year-old male. Biopsies were obtained after removal, to identify any underlying pathology.
Timing of endoscopic intervention is one of the most critical factors determining the eventual outcome. According to current ESGE and ASGE guidelines, procedures are classified time-wise as emergent (performed within 6 hours of patient presentation), urgent (performed in the first 24 hours) or nonurgent (performed electively within 48-72 hours). Overall, removal of a foreign object impacted in the oesophagus is recommended within 24 hours, even when only partial lumen obstruction has occurred [3,20].
Emergent endoscopic retrieval is recommended in cases of sharp pointed objects in the oesophagus, or when symptoms of complete oesophageal occlusion are present (i.e., drooling/inability to swallow fluids). Timely treatment reduces the risk of aspiration and perforation in these patients, as prolonged oesophageal impaction has been linked with increased incidence of complications. Furthermore, batteries and magnets ingestion warrant emergent retrieval, despite their blunt shape. Button batteries, when impacted in the narrower areas of the oesophagus may cause serious injury or even necrosis, due to electrical damage, pressure ischaemia and leakage of alkaline substances resulting in caustic injury. Cylindrical batteries are encountered more rarely and appear to be less dangerous, as they often move into the stomach, from where they can be removed even after 24 hours. Magnet ingestion in the upper GI tract must also be treated endoscopically within six hours, especially when concomitant ingestion of other magnets or metal objects is suspected, as the development of attraction between them might lead to incomplete or complete bowel obstruction, volvulus, pressure-induced ischaemia and perforation [3,6,20]. An algorithm summarising the proposed intervention timing and strategies in cases of foreign body ingestion is presented in Figure 2.

Figure 2. Proposed algorithm for foreign body ingestion management based on the latest ESGE and ASGE guidelines.
Pharmaceutical management with intravenous administration of glucagon has been used. Glucagon facilitates bolus passage into the stomach by acting as a smooth muscle relaxant. However, its efficacy is decreased in the context of underlying anatomic abnormalities and should not delay endoscopic intervention, which remains the treatment of choice [3,6,7,20,22].
Complications
Following initial management, patients with foreign body ingestion or food bolus impaction might be either admitted for further monitoring, or discharged and instructed as outpatients. In most cases, complications arise before endoscopic extraction and not as its result. Oesophageal perforation is the most common and severe complication. Following endoscopic extraction, perforations might be managed conservatively, although endoscopic treatment is indicated if recognised early. Surgical intervention will be required in rare cases. Hospitalisation is deemed appropriate after a technically challenging removal or in cases of failed endoscopic retrieval, especially when concerning sharp objects or batteries. Daily radiographic assessment is useful to monitor passing of the foreign body. Once into the colon, foreign body expulsion usually proceeds without problems and colonoscopy is rarely required [3,6,15].
CAUSTIC INGESTION
Epidemiology
Caustic ingestion refers to the consumption of a chemical substance that results in tissue injury on direct physical contact. These chemicals include a wide range of agents for domestic and industrial use, in the form of household cleaners, anti-rust agents, bleach, deodorants, batteries etc. [12,13]. Table 2 summarises the most common caustic substances encountered [13,26]. Frequently, the term corrosive is used as a synonym of caustic, although the first implies degradation, which is not always the case with caustic ingestion [13]. Nevertheless, in this review the two terms will be used interchangeably, for facilitation reasons.
According to the 2021 annual report of the American Association of Poison Control Center, there were nearly 50.000 cases of exposure to chemicals (acids: 7.325, alkalis: 3.471) and approximately 189.000 cases of household cleaning substances exposures. A significant number of these cases occurred by ingestion. The same report stated that in 2020 and 2021, household cleaning substances were the second most frequently consumed chemicals, both in adults and children [23].
Among the most common substances ingested in western countries, alkalis account for 79% of the total [8,12]. On the contrary, acid ingestion is more common in Asian regions like Iran, where hydrochloric acid is the most frequent cause of intentional ingestion [8]. The distinction between acids and alkalis is based on the pH (Potential of Hydrogen) of the corrosive agent.
Children aged five years or less represent the majority of cases worldwide (80%) and the remaining 20% is attributed to adolescents and adults [8,24]. Most minors consume unintentionally corrosive agents and have mild injuries. On the contrary, adults usually consume caustic chemicals in an attempt to commit suicide and present with more severe corrosive injuries. Most adult cases can be linked to psychiatric disorders, thus the evaluation of individuals by psychiatrists, should be an integral part of management [14,25].
Pathophysiology
Alkalis and acids produce tissue injury by different mechanisms. Alkalis tend to penetrate tissue by saponifying fats. The resultant injury is called liquefaction necrosis and is responsible for the formation of a gelatinous membrane which allows deep penetration and excessive damage to the mucosa. The injury extends rapidly through the wall of the oesophagus, towards the mediastinum, until tissue fluids buffer the alkalis. In the stomach the neutralisation of alkalis by gastric acid may limit the extent of injury. With that being said, consumption of a large volume and / or a high concentration alkaline solution, is expected to produce significant gastric injury [12,25,27-29].
The process of liquefaction necrosis lasts three to four days and results in vascular thrombosis and mucosal inflammation, excessive sloughing and formation of ulcers [30]. It is worth mentioning that the ingestion of ammonia, an alkali caustic agent, apart from the cited process above, leads to superficial haemorrhage of the stomach, 24 to 48 hours after the ingestion and requires strong suspicion from the treating physician [24].
In contrast, acids are responsible for the denaturation of proteins which results in coagulative necrosis. During this process, the consolidation of the connective tissue leads to the formation of oesophageal eschars which lessens tissue penetration and decreases the extent of injury. Despite this property, acid agents can cause severe injuries and death. As it passes through the stomach, the irritation of pylorus leads to pylorospasm and stagnation of the acid agent which results in injuries of the antrum and explains the sparing of duodenum in some cases [12,28,29].
Following caustic ingestion, either acid or alkali, the repair of the damaged tissue will start at approximately the end of the second week and the recovery will be completed by the sixth week. Around the third week, scars will start to form, a process that could last for several months and often advances to the formation of strictures. Figure 3 demonstrates the pathophysiological path following caustic ingestion.

Figure 3. The Pathophysiological Path After Caustic Ingestion.
A heavily scarred oesophagus demonstrates dysmotility problems that could lead to gastro-oesophageal reflux (GER) [31]. GER seems to further contribute to the formation of strictures and further decrease response to endoscopic dilation therapy [12].
Determinants of severity
The severity and extent of tissue injury after corrosive ingestion depends on multiple factors. The most important ones are the pH of the agent and the intent behind the ingestion. Other factors that should be considered are the physical form of the ingested agent (liquid, solid), the amount and concentration of the substance that is being consumed, the duration of contact with the tissue and the duration of time between consumption and medical treatment [33]. It is well established that pH values of <2 or >12 are considered as strong acids and alkalis respectively and translate into severe tissue injury. Acids tend to require longer contact time than alkalis in order to penetrate the tissue, so they ‘’prefer’’ the gastric mucosa from the oesophageal wall [11].
In case of massive ingestion of a highly concentrated agent, both acids and alkalis produce severe damage with excessive necrosis. The amount of ingestion is commonly linked to the intention behind the consumption [9]. Adults consume massive amounts of highly concentrated substances and delay to seek professional help with suicidal intent. On the contrary, children usually ingest small amounts with exploratory intent and usually spit them [34-38]. In conclusion, the intention behind the caustic ingestion and the pH of the substance seems to be the main risk factors and the main predictors of poor outcome [8].
Clinical presentation
The clinical signs and symptoms after corrosive ingestion vary widely depending on the location of the injury. The eyes, skin, airway, oesophagus, and stomach are the organs most likely involved. The injury may extend to adjacent tissues such as duodenum, jejunum, colon, pancreas, gallbladder but that is not frequently observed. The immediate and most frequently observed symptoms include pain, swelling of the tongue and mouth, dyspnea, dysphagia, hypersalivation, drooling, vomiting and self-limited hemorrhage in most cases [8]. Symptoms such as hoarseness, stridor and cough are indicative of epiglottic involvement, which could lead to respiratory failure, an indication for intubation. If oesophageal impairment is present dysphagia and odynophagia would most likely appear. Epigastric pain and bleeding are suggestive of gastric involvement. It is worth mentioning that symptoms do nοt correlate with the severity and extent of damage. The absence of pain and oral lesions does nοt rule out the possibility of severe oesophageal damage [12,24].
Complications
Among the short-term complications are oesophageal or gastric perforations. They can occur at any time, but usually present the first two to three weeks after the ingestion. Subcutaneous emphysema, retrosternal pain and haemodynamic instability should prompt a thorough evaluation for perforation. It is accompanied with high mortality as it could extend to mediastinum, causing mediastinitis, sepsis and subsequently death. Presence of gastric perforation will cause epigastric pain, rebound tenderness and signs of peritonitis. A sudden deterioration of a previously stable patient should prompt an emergency evaluation for perforation.
The delayed complications include the formation of strictures, fistulas with adjacent organs (aortoenteric fistulas, tracheoesophageal fistula), bleeding and oesophageal squamous cell carcinoma. By far the most common complication is the formation of strictures in the oesophageal lumen or at the pyloric antrum, usually 3 months to 1 year after the caustic ingestion. Corrosive strictures of the oesophagus are commonly multiple, long, irregular and have long stabilisation delays. Symptoms related to oesophageal strictures are substernal pain, dysphagia and odynophagia. Gastric strictures are rare because of the large diameter of the stomach, but the formation of strictures at the area of the gastric antrum is responsible for gastric outlet obstruction syndrome, which causes early satiety, post- prandial nausea, vomiting and weight loss. Collectively, stricture formation is a disabling and resource consuming issue, which affects the quality of life [12,29,39].
Bleeding is an unusual late sequela after corrosive ingestion. In most cases, it is a single, self-limiting event, although severe haemorrhage has been reported. The formation of fistulas with adjacent organs is a very rare phaenomenon (its occurrence is less than 3%) but the mortality rates are very high when aortoenteric fistulas are present. They can occur at any time after ingestion [24,40]. Lastly, patients after caustic ingestion, demonstrate a 1000-to-2000-fold increase in the incidence of oesophageal carcinoma, but this risk may be overestimated [25,29,42]. Nevertheless, it is prudent to implement endoscopic surveillance. A surveillance protocol dictating endoscopy at 2–3-year intervals, starting 20 years after the caustic ingestion has been proposed [29,42].
Diagnosis
Laboratory tests
At the emergency department a complete blood count and full biochemical screening tests with measurement of electrolytes, creatinine, liver tests, CRP (C-reactive protein), pH, serum lactate, blood alcohol level and β-HCG, in young women, should be performed. Blood test results are not directly correlated to the severity of damage and normal values cannot rule out significant oesophageal or gastric damages [12,42]. However, monitoring the pattern of change of blood test values contributes to a patient’s management protocol, with severe acidosis, elevated WBC and CRP, deranged liver tests, thrombocytopenia and renal failure suggesting severe damage [11,14,24,42]. It is worth highlighting that specific agents are known to cause severe electrolyte disturbances (hypocalcaemia: phosphoric, hydrofluoric acids/ hyponatraemia: strong alkalis and acids/ hypokalaemia,etc.), which could further deteriorate a patient’s outcome [14].
Risk stratification
For decades, endoscopy has been the main tool in the evaluation algorithms. The main drawback is its inability to accurately predict depth of necrosis, which could result in unnecessary or delayed surgery. Recently, in 2019, the role of CT imaging for risk stratification of caustic ingestions by the World Society of Emergency Surgery consensus (WSES) conference was also proposed as an alternative [14].
Endoscopic evaluation
Flexible endoscopy when used should not be delayed. It should be performed ideally in the first 3-48 hours to reduce the danger of endoscopy-associated complications (i.e. perforation) and to avoid misinterpretation due to mucosal changes. The Zargar classification is the most widely used grading system [45]. The endoscopic classification of corrosive injuries along with their prognosis is summarised in Table 3 [46]. The extent of oesophageal damage on endoscopy is a predictor of complications, with a nine-fold increase in mortality and morbidity for every increased grade [42]. Generally, patients with endoscopic grade 3b or more, will need emergency surgery, whereas patients with grade 3a or less could be managed non operatively [14]. Endoscopy remains the main diagnostic and therapeutic tool for oesophageal or gastric strictures.
Endoscopic ultrasound (EUS) has been used to evaluate the extent of damage of the oesophageal muscular layers and consequently, it could predict the formation of strictures. However, it failed to outperform conventional endoscopy in predicting early or late complications. For now, there is no place in guidelines for EUS but further research is needed [43-44].
Imaging evaluation
A plain chest radiograph in the upright position is the initial test in most patients, but demonstrates low sensitivity and specificity. When disclosing free air in the abdomen it should prompt for further evaluation [43-44].
CT, much like endoscopy, should also be performed as soon as possible, preferably in the first 3-6 hours following caustic ingestion. CΤ of the neck, thorax and abdomen can accurately evaluate the extent of injury, predict patients in need of surgical treatment and forecast the early/late consequences [14]. The radiological classification based on CT findings is demonstrated in Table 4 [25]. According to this three-fold grading system, the absolute absence of enhancement of the organ’s wall after the injection of an intravenous iodine-based contrast agent is indicative of transmural necrosis and should prompt for emergency treatment [24].
The choice between endoscopy or/and CT should be based on local availability and expertise. There is no clear consensus. Although both modalities are widely available, there is considerably greater experience with endoscopy. CT evaluation is based on bowel ischaemia protocols and although results can be reproduced by outside expert centers, it requires radiologists that are familiarised with this protocol. Endoscopy is useful in cases that CT cannot be performed or is contraindicated (CT is unavailable, patient history of allergic reaction to iodine-based contrast agents, inconclusive results and children) [14]. CT offers the advantage of being less invasive and thus it can be utilised better in patients with more severe clinical presentation, especially when there is a strong suspicion of perforation. An individualised approach is advised [12,14,24].
Management
Initial approach should align with the Acute Life Support (ATLS) guidelines for burn injuries. This includes securing the airway, administering pain relief medicine and establishing haemodynamic stabilisation with intravenous fluid resuscitation. The Poison Control Center should be contacted as soon as possible to evaluate the toxicity of the agent and guide treatment. Following caustic ingestion, the most life-threatening event is loss of the airway due to oedema and direct impairment of the larynx. The threshold for placement of a definitive airway should be low in the presence of symptoms suggestive of airway obstruction (stridor, inability to control secretions, hoarseness, loss of consciousness, etc.). It is preferable to use a guided fiberoptic laryngoscope over blind intubation to avoid further injuries to the upper airway. It is of paramount importance to prevent vomiting and repeated passings of the caustic agent through the oesophagus in order to minimise damage. The patient should be placed in a 45-degree position and receive antiemetic medicines, such as metoclopramide. The insertion of a nasogastric tube is not recommended because it could result in further damage, by leading to gagging and vomiting, further exposing the oesophagus to the corrosive agent. Moreover, it is contradicted to administer pH neutralisation agents because they lead to exothermic reactions, contributing to more injury [25]. Administration of milk or charcoal has never been proven and is not advised [12]. The use of PPIs or H2- blockers is advised [25,32].
The use of corticosteroids is controversial. Most studies failed to show a benefit of prolonged administration of a high dose of a corticosteroid, so their use is contradicted unless the patient demonstrates symptoms of upper airway involvement [12,24-25,42]. However, Usta and colleagues support the administration of a 3-day course of methylprednisolone, as it seems to limit the formation of strictures, in children’s population, after alkaline ingestion [47]. Based on the above, a short-term administration of steroids, to patients with alkaline grade 2b on the endoscopic classification, could be beneficial but more research is required [13]. Use of antibiotics is not routinely recommended unless indicated (i.e., infection) [25,42].
After initial evaluation, most patients (70%-90%) will be deemed eligible for non-operative treatment. If the following values are present: grade I on CT, consumption of a small amount, low concentration of the agent and the patient is able to control saliva/ no symptoms of airway obstruction, it is safe to discharge the patient after a brief observational time. In all other cases, fasting is mandatory and the patient should be closely observed for at least 48 hours after the ingestion [14].
Most patients with grade 3 on CT classification, or grade 3b on endoscopic classification, especially those with clinical signs of perforation/peritonitis and haemodynamic instability, should be treated with emergency surgery. Laparotomy remains the standard approach and transhiatal stripping oesophagectomy with total gastrectomy is the most commonly used procedure. All organs that show transmural necrosis should be resected at the emergency surgery. Signs and symptoms suggesting ongoing necrosis should prompt an evaluation with a second CT and maybe additional surgery [14,25].
Management of strictures
The most common late sequelae after corrosive ingestion, is the appearance of strictures. Endoscopy (dilations) remains the first-line of non-operative treatment and the upfront tool for the evaluation of symptomatic patients. It should be avoided in the first 5-15 days after caustic ingestion because the tissue is friable during the healing period and perforation could occur easily [29,42]. Both balloon dilators and bougies have been used, with no clear advantage of each method over the other. Usually multiple sessions (3-5) will be required in order to successfully create sufficient luminal conduit. The intervals between sessions vary from 1 week to 3 weeks. The use of stenting for oesophageal dilation is still being researched and more data are required in order to determine the optimal time and the type of stent most suitable [14]. After 5-7 failed attempts, reconstruction surgery of the oesophagus should be considered.
CONCLUSION
In conclusion, although foreign body ingestion and food bolus impaction are frequently encountered and are usually self-resolved conditions, their management requires a multidisciplinary approach by a team consisting of gastroenterologists, otorhinolaryngologists, surgeons and radiologists, in order to diagnostically confront complications and achieve the optimal therapeutic result. Oesophageal involvement, especially of the upper third, constitutes a true endoscopic emergency. Flexible endoscopy is the treatment of choice in these cases, with excellent safety and efficacy. Gastroenterological societies’ guidelines recommend the establishment of secondary re-evaluation in all patients, aiming to recognise latent pathologic conditions and prevent symptom recurrence.
Consumption of corrosive agents remains a significant public health problem, with increasing numbers in developing countries. Despite the high morbidity and mortality, it is widely unreported, a factor that hinders the formation of guidelines. As caustic agents can be found in an enormous amount of household products, the main future directions should focus on prevention of injury with safe packaging regulations and educational programs. CT and endoscopy are the cornerstones of the emergency evaluation after caustic ingestion. An individualised approach based on the severity of the case and the local expertise is necessary. Endoscopic dilation is the upfront non-operative treatment of strictures, which are the most commonly observed late consequence. Surgery is recommended in all patients who demonstrate transmural necrosis and in cases that endoscopic dilation fails to establish sufficient oesophageal patency.
Conflict of interest disclosure: None to declare
Declaration of funding sources: None to declare
Author contributions: All authors contributed equally to the current work.
REFERENCES
- Jayachandra S, Eslick GD. A systematic review of pediatric foreign body ingestion: presentation, complications, and management. Int J Pediatr Otorhinolaryngol. 2013;77(3):311–7.
- Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep. 2005;7(3):212–8.
- Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(5):489–96.
- Ko HH, Enns R. Review of food bolus management. Can J Gastroenterol. 2008;22(10):805–8.
- Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55(7):802–6.
- Becq A, Camus M, Dray X. Foreign body ingestion: dos and don’ts. Frontline Gastroenterol. 2021;12(7):664–70.
- Ambe P, Weber SA, Schauer M, Knoefel WT. Swallowed foreign bodies in adults. Dtsch Arztebl Int. 2012;109(50):869–75.
- Faz AA, Arsan F, Peyvandi M, Oroei M, Shafagh O, Yousefi M, et al. Epidemiologic Features and Outcomes of Caustic Ingestions; a 10-Year Cross-Sectional Study [Internet]. Vol. 5, Emergency. 2017. Available from: www.jemerg.com
- Chirica M, Resche-Rigon M, Bongrand NM, Zohar S, Halimi B, Gornet JM, et al. Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg. 2012;256(6):994–1001.
- Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41(1):33–8.
- Le Naoures P, Hamy A, Lerolle N, Métivier E, Lermite E, Venara A. Risk factors for symptomatic esophageal stricture after caustic ingestion-A retrospective cohort study. Dis Esophagus. 2017;30(6):1-6.
- Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: A comprehensive review. World J Gastroenterol. 2013;19(25):3918–30.
- Hoffman RS, Burns MM, Gosselin S. Ingestion of Caustic Substances. N Engl J Med. 2020;382(18):1739–48.
- Chirica M, Kelly MD, Siboni S, Aiolfi A, Riva CG, Asti E, et al. Esophageal emergencies: WSES guidelines. Vol. 14, World Journal of Emergency Surgery. BioMed Central Ltd.; 2019.
- Bekkerman M, Sachdev AH, Andrade J, Twersky Y, Iqbal S. Endoscopic Management of Foreign Bodies in the Gastrointestinal Tract: A Review of the Literature. Gastroenterol Res Pract. 2016;2016:8520767.
- Kim JH, Lee DS, Kim KM. Acute appendicitis caused by foreign body ingestion. Ann Surg Treat Res. 2015;89(3):158–61.
- Yao C-C, Wu I-T, Lu L-S, Lin S-C, Liang C-M, Kuo Y-H, et al. Endoscopic Management of Foreign Bodies in the Upper Gastrointestinal Tract of Adults. Biomed Res Int. 2015;2015:658602.
- Sugawa C, Ono H, Taleb M, Lucas CE. Endoscopic management of foreign bodies in the upper gastrointestinal tract: A review. World J Gastrointest Endosc. 2014;6(10):475–81.
- Young CA, Menias CO, Bhalla S, Prasad SR. CT features of esophageal emergencies. Radiographics. 2008;28(6):1541–53.
- ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73(6):1085–91.
- Asge Technology Committee, Diehl DL, Adler DG, Conway JD, Farraye FA, Kantsevoy SV, et al. Endoscopic retrieval devices. Gastrointest Endosc. 2009;69(6):997–1003.
- Schupack DA, Lenz CJ, Geno DM, Tholen CJ, Leggett CL, Katzka DA, et al. The evolution of treatment and complications of esophageal food impaction. United Eur Gastroenterol J. 2019;7(4):548–56.
- Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Rivers LJ, Feldman R, et al. 2021 Annual Report of the National Poison Data System© (NPDS) from America’s Poison Centers: 39th Annual Report. Clin Toxicol (Phila). 2022;60(12):1381–643.
- Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. 389, The Lancet. Lancet Publishing Group; 2017. p. 2041–52.
- Bonavina L, Chirica M, Skrobic O, Kluger Y, Andreollo NA, Contini S, et al. Foregut caustic injuries: results of the world society of emergency surgery consensus conference. World J Emerg Surg. 2015;10(1):44.
- Maskati QB, Maskati BT. Management of chemical injuries of the eye. Indian J Ophthalmol. 1987;35(5–6):396–400.
- Cello JP, Fogel RP, Boland CR. Liquid caustic ingestion. Spectrum of injury. Arch Intern Med. 1980;140(4):501–4.
- Fisher RA, Eckhauser ML, Radivoyevitch M. Acid ingestion in an experimental model. Surg Gynecol Obstet. 1985;161(1):91–9.
- Keh SM, Onyekwelu N, McManus K, McGuigan J. Corrosive injury to upper gastrointestinal tract: Still a major surgical dilemma. World J Gastroenterol. 2006;12(32):5223–8.
- Gumaste V V, Dave PB. Ingestion of corrosive substances by adults. Am J Gastroenterol. 1992;87(1):1–5.
- Mutaf O, Genç A, Herek O, Demircan M, Ozcan C, Arikan A. Gastroesophageal reflux: a determinant in the outcome of caustic esophageal burns. J Pediatr Surg. 1996;31(11):1494–5.
- Cakal B, Akbal E, Köklü S, Babalı A, Koçak E, Taş A. Acute therapy with intravenous omeprazole on caustic esophageal injury: a prospective case series. Dis esophagus Off J Int Soc Dis Esophagus. 2013;26(1):22–6.
- Goldman LP, Weigert JM. Corrosive substance ingestion: a review. Am J Gastroenterol. 1984;79(2):85–90.
- Temiz A, Oguzkurt P, Ezer SS, Ince E, Hicsonmez A. Predictability of outcome of caustic ingestion by esophagogastroduodenoscopy in children. World J Gastroenterol. 2012;18(10):1098–103.
- Riffat F, Cheng A. Pediatric caustic ingestion: 50 consecutive cases and a review of the literature. Dis esophagus. 2009;22(1):89–94.
- Betalli P, Falchetti D, Giuliani S, Pane A, Dall’Oglio L, de Angelis GL, et al. Caustic ingestion in children: is endoscopy always indicated? The results of an Italian multicenter observational study. Gastrointest Endosc. 2008;68(3):434–9.
- Cheng H-T, Cheng C-L, Lin C-H, Tang J-H, Chu Y-Y, Liu N-J, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008;8:31.
- Chang J-M, Liu N-J, Pai BC-J, Liu Y-H, Tsai M-H, Lee C-S, et al. The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol. 2011;11:72.
- Hugh TB, Kelly MD. Corrosive ingestion and the surgeon. J Am Coll Surg. 1999;189(5):508–22.
- Tseng Y-L, Wu M-H, Lin M-Y, Lai W-W. Massive upper gastrointestinal bleeding after acid-corrosive injury. World J Surg. 2004;28(1):50–4.
- Kirsh MM, Ritter F. Caustic ingestion and subsequent damage to the oropharyngeal and digestive passages. Ann Thorac Surg. 1976;21(1):74–82.
- Lusong MAA De, Timbol ABG, Tuazon DJS. Management of esophageal caustic injury. World J Gastrointest Pharmacol Ther. 2017;8(2):90.
- Kamijo Y, Kondo I, Kokuto M, Kataoka Y, Soma K. Miniprobe ultrasonography for determining prognosis in corrosive esophagitis. Am J Gastroenterol. 2004;99(5):851–4.
- Chiu H-M, Lin J-T, Huang S-P, Chen C-H, Yang C-S, Wang H-P. Prediction of bleeding and stricture formation after corrosive ingestion by EUS concurrent with upper endoscopy. Gastrointest Endosc. 2004;60(5):827–33.
- Zargar SA, Kochhar R, Mehta S, Mehta SK. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37(2):165–9.
- Bruzzi M, Chirica M, Resche-Rigon M, Corte H, Voron T, Sarfati E, et al. Emergency Computed Tomography Predicts Caustic Esophageal Stricture Formation. Ann Surg. 2019;270(1):109–14.
- Usta M, Erkan T, Cokugras FC, Urganci N, Onal Z, Gulcan M, et al. High doses of methylprednisolone in the management of caustic esophageal burns. Pediatrics. 2014;133(6):E1518-24.