ACHAIKI IATRIKI | 2021; 40(1):38–43
Original research article
Christos Bartsokas, Eleni Jelastopulu
Department of Public Health, School of Medicine, University of Patras, University Campus, Rio, Greece
Received: 01 Oct 2020; Accepted: 22 Dec 2020
Corresponding author: Christos Bartsokas, Department of Public Health, School of Medicine, University of Patras, 26500 Rio, Greece, Tel.: +30 2610 969878, Fax: +30 2610 996101, E-mail: bartsokas@gmail.com
Key words: Inequality, health care, primary care sector, hospital sector
Abstract
Background: Accessibility in health care defines a universal health system. Our goal was to investigate the equality on the distribution of health resources, in the middle of economic crisis, between hospitals and primary care sector in the Western Greece region.
Methods: All data were provided by the Hellenic Statistical Authority for the years 2010 to 2013. Gini coefficients were calculated in order to measure inequality, ranging from 0 to 1, where 1 stand for the absolute inequality. Calculations were based on population size and geographic size, respectively, for the indicators: number of institutions, health workers and hospital beds.
Results: Distribution of health resources for hospital and primary care sector were reported for each prefecture in the Western Greece region separately and as a whole. The urban prefecture of Achaia demonstrated higher rates of resources in hospital sector, inversely more rural ones have had higher rates in primary health care resources. Gini coefficient ranged between 0.40 to 0.49 for hospitals, while in the primary care sector it was around 0.21, indicating a good equality in the distribution of resources.
Conclusion: Amidst economic crisis for Greece, inequality in the geographic distribution of health resources was evident, despite a more equitable per population distribution of resources. In the urban prefecture of Achaia, it is more likely to have access to well-resourced hospitals for outpatient care, while the lower rates of health resources in the primary care sector depict chronic systemic disparities. A focus on resources needed for specific health services will contribute to dealing with inequalities in order to achieve a universal health system.
Introduction
Universal health systems aim to provide health care for all, or to rephrase it, they aim on equal distribution of health resources based on peoples’ needs [1,2]. Healthcare resources are defined as all materials, personnel, facilities, funds, and anything else that can be used for providing health care services. Equity in resource distribution requires that individuals with the same need have access to the same resources (horizontal equity) and that individuals with greater need have access to more resources (vertical equity). In 2010, WHO reported as one of the main barriers to universal health coverage the availability and inequitable use of resources [3].
In Greece, healthcare services are delivered by primary care institutions and hospitals. Primary care institutions which mainly focus on preventive health practices, seem to lack resources compared with hospitals treating medical conditions. Thus, more resources have been poured into hospitals, further exacerbating disparities between hospitals and primary care institutions [4,5]. In a generalized framework, the economic crisis which started in 2008, deepened inequalities in almost all aspects of social life [6] and had a negative influence on population health, especially mental health [7,8]. This is partly due to the psychological insecurity, stress and access to material goods, and partly as a consequence of lack of access to healthcare.
In the past, several studies have shown inequity in healthcare resources regarding specific health conditions [9]; or in a specific health care delivery system [10]. In our study, we investigated the differences in the distribution of healthcare resources between the primary health sector and hospitals in a Greek region in regard with geographic location and population size. This study’s results can inform policy makers on how these resources are distributed among Western Greece, a region with one of the lowest gross domestic product in Greece [11]. Furthermore, since no previous study has dealt with the issue in Greece, the findings of the present study provide appropriate evidence for the future planning and management of health sector resources in order to improve access to health services in the country.
Methods and materials
Data were extracted by the Hellenic Statistical Authority for the time period between 2010 to 2013 [12]. Population and geographic size were reported for Western Greece as a whole and by prefecture. A detailed statistical yearbook included exclusively public hospitals and primary health centres along with information about the number of institutions and number of available beds and health workers per institution, reflecting health resources.
We used Gini coefficient as the indicator for mea-suring inequality in the distribution of health resources against population size and geographic area. This index calculation is based on Lorenz curve (Figure 1), which is a graphical representation of the cumulative proportion of health resources against the cumulative proportion of geographic area or population size. Pivotal properties of Lorenz curve are, that it always starts at (0,0) and ends at (1,1) and cannot rise above the line of perfect equality of 450. It defines two areas in the level, area A, the area between the line of perfect equality and the observed Lorenz curve and area B, the one between the Lorenz curve and the line of perfect inequality. Thus, the Gini coefficient is the ratio of the area between the line of perfect equality and the observed Lorenz curve to the area between the line of perfect equality and the line of perfect inequality. We have used this formula for calculating Gini coefficient:
Gini coefficient = area A/(area A + area B)
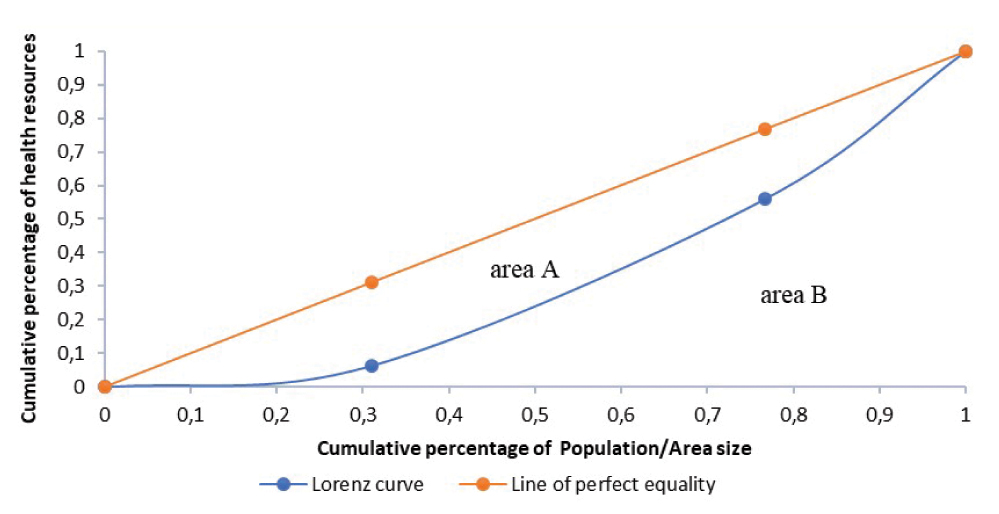
Figure 1. The straight line (orange line) depicts the line of perfect equality where resources are distributed evenly, while the curved line (blue line) shows the actual distribution of resources, giving a graphic representation of existed distribution inequality
Therefore, it could take values from 0 to 1. The higher the coefficient, the more unequal the distribution is. Thus, Gini coefficient values categorised as absolute equality (GI <0.2), high equality (GI=0.2-0.3), inequality (GI=0.3- 0.4), high inequality (GI=0.4-0.6) and absolute inequality (GI >0.6) [13]. All data were analysed using SPSS v.25.0
Results
Tables 1 and 2 show the distribution of health resources for hospitals and the primary care sector, respectively. The Achaia prefecture, the most developed one in the region, had a much higher density in the distribution of hospitals, beds and health workers in the hospital sector, while a more equitable distribution compared with other prefectures in the distribution of heath resources in the primary care sector. In addition, the Ilia and Etoloakarnania prefectures, reported a much lower distribution of resources in the hospital sector while in the primary care sector we had a relatively inversed picture with increasing rates of resources in both rural prefectures compared with the Achaia prefecture, which could be categorized as more industrialised.
Table 3 depicts that the Gini coefficients against population size ranged between 0.04 and 0.21 in the hospital sector: 0.21 for the number of hospitals, around 0.14 for the number of beds and 0.04 for the number of health workers, respectively, indicating a good equality. The primary care sector showed a slightly higher level of Gini coefficients. The distribution in the number of primary health care institutions, beds and health workers was equitable, with Gini coefficients ranging from 0.21 to 0.34.
No trend was found in Gini coefficients over the years from 2010 to 2013. However, relative inequality was evident in the geographic distribution of health resources in hospitals. The Gini coefficients were between 0.40-0.49 in the geographic distributions of institutions, health workers and beds, indicating a higher level of inequality. The geographic distribution of primary care centres was equitable.
Discussion
In our study, we investigated inequality in the distribution of health resources of hospital and primary sector in Western Greece, by using Gini coefficient. We found that inequality exists per geographic distribution of health resources in hospitals. We did not detect inequality either in the primary care sector or per population size. Health inequalities are generally understood to refer to differences in health between groups of people who are better or worse off socioeconomically, as reflected, for example, by their occupational status, income level, expenditures, wealth, or education, or by the economic characteristics of the places where they live. They are unfair and should be reduced by the right mix of government policies.
Not finding inequality in the primary care sector is not surprising, given that most resource planning programs have taken into consideration population size [14] and several reforms have been proposed since 1998 in the primary health care sector. Since Western Greece is a region with a medium geographic size but with the lowest Gross Domestic Product (GDP), defined as a standard measure of the value added created through the production of goods and services in an area during a certain period, in the country, this makes our results even more indicative of Greece’s health related policies during the economic crisis [11,15].
Previous research in the field has demonstrated that a region with a high density of fairly distributed healthcare workforce is more likely to serve the healthcare needs of its people than a region with a low workforce density [16]. This can be seen in the primary sector in western Greece but not in hospitals per geographic size, probably due to the fact that despite their problems, the Greek primary healthcare centres represent the only organisational structure able to offer holistic services to clearly defined local populations [17]. While an equal distribution of beds and number of health care facilities (in both hospital and primary care centers) is documented in the literature, the number of healthcare professionals shows a much lower density in the primary care sector compared to the hospital sector, depicting thus the dominant role of the hospital sector in the Greek healthcare system [18-20].
In the present study, we focused on inequalities in health resources allocation and comparisons between the primary and the hospital sector. Existing literature is lacking information regarding those inequalities; we found only two studies from China and Ethiopia, pointing out inequalities between health system levels [18,21] and only the latter exclusively in the public health sector as it is stated in the present study. Similarly to our results, a much more developed hospital sector was prominent in China. Although some progress had been made with increased governmental investments in primary care, the capacity development of primary care still lags behind the hospital sector. Several other studies in China also found that quality resources tend to be increasingly concentrated in hospitals. In addition, as shown in our study, internal disparities within each economic zone further illustrate the regional differences in the equality of healthcare. The urban prefecture of Achaia has a much higher level of inequality compared with the other regions. Other studies tried to simplify the complexity in the nature of healthcare expenses distribution and revealed that high income countries demonstrated a lower intra-regional inequality compared with lower income ones [21,22], recognizing healthcare expenses as pivotal in minimizing inequalities.
A reduction in public spending in Greece between the years 2009 to 2013 by 30% deepened the gap between preventive medicine policies and curing diseases [23]. Thus, policies to support primary health care and decongest hospitals will strengthen the national health system instead of creating the impression of a two-tier system that opposes each other. More specifically, more health resources, especially quality health workers, should be allocated to primary care institutions in order to narrow the capacity gap between hospitals and primary care institutions. Secondly, regional disparities need to be addressed. This can only be done through financial transfer coordinated by the central government. The current governmental budgeting system and the social health insurance arrangements in Greece are highly centralized and tethered, preventing the central government from fulfilling this role [24].
This study has some limitations as it analysed only a short period of time, in the middle of economic crisis. It would be interesting to perform further analyses on the longer-term changes, not only in Western Greece but throughout the country, when data are made available. We have selected those health resources indicators based on the availability by Hellenic Statistical Authority.
Conclusions
The proper and fair distribution of health resources, hospitals, beds and manpower, has a crucial role in delivering healthcare services. Inequality was found for health resources in the hospital sector in regard with geographic distribution, despite a more equitable per capita distribution of resources. The distribution of the primary health sector resources in Western Greece demonstrated a good equality, too. In addition, an existing gap in resources rates between urban and rural prefectures, was revealed; depicting the fact that people living in an urban area are more likely to use well-resourced hospitals than people living in rural areas. Further research should identify inequalities in resources needed for the deliverance of specific health services. In this way, the adjustment of specific healthcare policies will lead to a fairly equal distribution of health resources as a milestone in the development of a universal healthcare system.
Conflict of interest disclosure: None to declare.
Declaration of funding sources: None to declare.
Author contributions: Christos Bartsokas: conception and design; analysis and interpretation of the data; drafting of the article; critical revision of the article for important intellectual content; final approval of the article, Eleni Jelastopulu: conception and design; critical revision of the article for important intellectual content; final approval of the article.
References
- Daniels N, Kennedy BP, Kawachi I. Why justice is good for our health: the social determinants of health inequalities. Daedalus 1999;128(4):215–251.
- Feinberg J. Encyclopedia of Bioethics: Justice. New York: Macmillan; 1995.
- World Health Organization. The world health report Health systems financing: the path to universal coverage. Geneva: The World Health Organization; 2010. Available from: https://www.who.int/whr/2010/en/
- Lionis C. Primary care in Greece. European forum for primary care; 2011.
- The National Organization for the Provision of Health Services (Greek acronym EOPYY). Available from: https://eu-healthcare.eopyy.gov.gr/en/2_1.aspx
- Karanikolos M, Kentikelenis A. Health inequalities after austerity in Greece. International Journal for Equity in Health. Int J Equity Health. 2016;15:83.
- Bouras G, Lykouras L. The economic crisis and its impact on mental health. Encephalos. 2011;48:54-61
- Karamanoli E. Debt crisis strains Greece’s ailing health system. Lancet. 2011;378(9788):303–304.
- Yuan S, Hong Y, Klemetti R, Qiang L, Shengbin X, Jianmin G, et al. Equity in use of maternal health services in western rural China: a survey from Shaanxi province. BMC Health Serv Res. 2014;14:155.
- Ameryoun A, Meskarpour-Amiri M, Dezfuli-Nejad ML, Khoddami-Vishteh H, Tofighi S. The assessment of inequality on geographical distribution of non-cardiac intensive care beds in Iran. Iran J Public Health. 2011;40(2):25-33.
- Organisation for Economic Co-operation and Development. Regions and Cities in Greece; 2018. Available from: https://www.oecd.org/cfe/GREECE-Regions-and-Cities-2018.pdf
- Hellenic Statistical Authority. Digital Library. Available from: http://dlib.statistics.gr/portal/page/portal/ESYE/
- Miao CX, Zhuo L, Gu YM, Qin ZH. Study of large medical equipment allocation in Xuzhou. J Zhejiang Univ Sci B. 2007;8(12):881-4.
- Lostao L, Blane D, Gimeno D, Netuveli G, Regidor E. Socioeconomic patterns in use of private and public health services in Spain and Britain: implications for equity in health care. Health Place. 2014;25:19-25
- Administrative Regions of Greece. Available from: https://en.wikipedia.org/wiki/Administrative_regions_of_Greece
- Anand S. Measuring health workforce inequalities: methods and application to China and India. World Health Organization; 2010. Available from: https://apps.who.int/iris/handle/10665/44417
- Benos A. Primary health care by 2000. latrika Themata. 1999;16:12–15.
- Zhang T, Xu Y, Ren J, Sun L, Liu C. Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health. 2017;16(1):42.
- Stordeur S, Leonard C. Challenges in physician supply planning: the case of Belgium. Hum Resour Health. 2010;8:28.
- Boutsioli Z. The Greek Hospital Sector and Its Cost Efficiency Problems in Relation to Unexpected Hospital Demand: A Policy-making Perspective. Rev Eur Stud 2010;2:170.
- Woldemichael A, Takian A, Sari A, Olyaeemanesh A. Inequalities in healthcare resources and outcomes threatening sustainable health development in Ethiopia: panel data analysis. BMJ Open 2019;9(1):e022923
- Lessmann C. Regional inequality and decentralization: an empirical analysis. Environment and Planning A 2012;44(6):1363–88.
- Organisation for Economic Co-operation and Development. Health Policy in Greece; 2016. Available from: http://www.oecd.org/greece/Health-Policy-in-Greece-January-2016.pdf
- Skalli A, Johansson E, Theodossiou I. “Are the Healthier Wealthier or the Wealthier Healthier? The European Experience”, Helsinki: ETLA. The case of Greece; 2006