ACHAIKI IATRIKI | 2021; 40(2):107–110
Case Report
Ioannis Vogiatzis, Konstantinos Koutsampasopoulos, Pavlos Roditis
Department of Cardiology, General Hospital of Veroia, Veroia, Greece
Received: 13 May 2020; Accepted: 11 Jul 2020
Corresponding author: Dr Ioannis Vogiatzis, Director of Department of Cardiology, General Hospital of Veroia, 59100 Veroia, Tel/Fax: +30 2331359253 +30 6944 276230, E-mail: ivogia@hotmail.gr
Key words: Spontaneous, coronary artery dissection, healing
Abstract
Spontaneous coronary artery dissection is an uncommon cause of myocardial infarction. Young healthy women are most frequently affected. Dissection of the left main coronary artery is even less common; only 18 cases have been reported. We describe the case of a 45-year-old male who presented in our hospital in a stable condition with Spontaneous coronary artery dissection (SCAD) extending in the middle of the Left Anterior Descending (LAD) after coronary angiography. Coronary angiography performed 6 months later, showed complete angiographic healing. The indicated therapeutic approach to hemodynamically stable patients is conservative with spontaneous angiographic healing. SCAD is a potential diagnosis in patients, especially females, presenting with symptoms of acute coronary syndromes.
Introduction
Spontaneous coronary artery dissection (SCAD) is a rare, non-atherosclerotic cause of acute coronary syndromes (ACS) (1.7-4% in recent series) [1]. SCAD is caused by the sudden disruption of the coronary artery wall, resulting in separation of the inner intimal lining from the outer vessel wall [2]. Advances in imaging techniques and better recognition of SCAD have led to several new insights into this understudied condition [3]. The treatment is interventional [Percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)] or conservative, depending on the occurrence of extensive ischemia, heart failure or potentially life-threatening ventricular arrhythmias. A variety of stressors (emotional or physical) trigger-mechanisms are responsible for the dissection, as they weaken the arterial wall [4].
We describe the case of a forty-five-year-old male with severe SCAD which resolved spontaneously after six months without any further interventional treatment.
Case description
A 45-year-old man was admitted to our hospital for coronary angiography (CA) and possible PCI after 48 hours of ACS. He was stable with a heart rate of 72beats/min, blood pressure of 145/95mmHg and oxygen saturation of 99% in room air. He was asymptomatic, without any sign of ischemia in the ECG. Furthermore, the ECG showed ST-segment elevation in leads V3-V5 (Figure 1), hs-troponin blood level was 4.1ng/ml at admission (this was the peak troponin value) and chest X-ray (CxR) was clear. He reported that he was an athlete of isometric exercises (weight-lifting). However, the event was not associated with any sport activity.
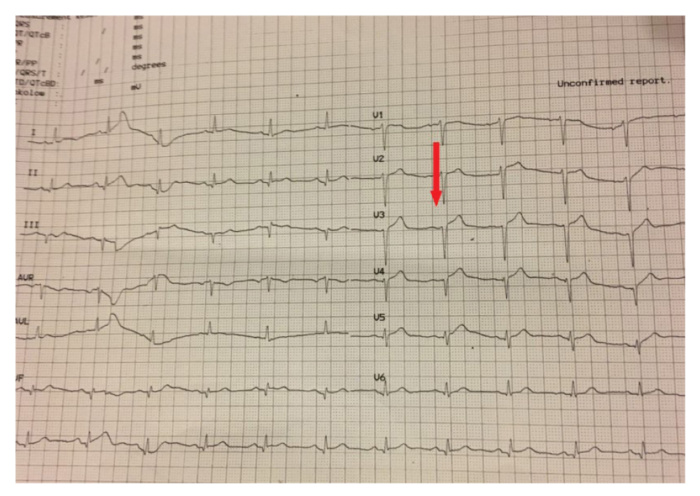
Figure 1. ECG showed an ST-elevation at V3, V4, V5 leads (Arrow).
He had no past medical history or any medication history. The patient’s clinical picture pertains to the time he was transferred to our hospital for coronary angiography, 48 hours after the initial administration.
CA was performed showing a type I dissection extending in the middle of the left anterior descending (LAD) (Figure 2A, 2B). No other coronary stenoses or abnormalities were observed. Given that he was clinically stable without any symptoms, we decided to abandon any further coronary intervention and to perform a simple follow up. The following day, the patient was discharged on aspirin, clopidogrel, atorvastatin and metoprolol.

Figure 2. Coronary Arteriography (CA) in successive time intervals showing the spontaneous dissection and the spontaneous late healing. A: 48 hours after the presentation (29/3/2016). The arrow points to dissection in the middle portion of the Left Anterior Descending (LAD) Artery. B: Image from the same CA showing the true and the false lumens. C: Image 4 months after the initial. The arrow shows the LAD artery with the same dissection. D: Image from a repeated CA 6 months after the initial presentation (30/9/2016). The arrow points to the region with the previous dissection which spontaneously had healed with the restoration of normal coronary flow.
The patient discontinued exercise and after 3 months a new CA was performed with precisely the same results. (Figure 2C).
However, after 6 months from the first episode, the followed CA finally showed complete spontaneous healing, without any sign of dissection (Figure 2D).
Discussion
In the present case, even this severe SCAD healed spontaneously without any interventional treatment. We followed up the case with repeated CA every 3 months to check the condition and to decide follow-up therapy. The dissection was spontaneously healed after six months and this proves that any aggressive interventional treatment strategy should be reconsidered since it induces more complications than benefits in stable patients with SCAD.
Conservative management in stable SCAD patients without evidence of ongoing ischemia features a good overall prognosis with the majority showing spontaneous healing of the dissection on follow-up angiography, which is concordant with our patient. When a spontaneous coronary dissection is presented, with no sign of ischemia, it is recommended a follow-up with a conservative strategy [5]. It is scientifically proven that in most cases, probable revascularization is associated with significantly increased failure rates and complications [2]. Revascularization is restricted to patients with hemodynamic instability or ongoing ischemia.
SCAD is estimated to be responsible for 0.1 to 0.4% of all ACS cases. It is an important cause of ACS in young women, responsible for up to 25% of all ACS cases in women <50 years of age and up to 25% of cases diagnosed during the peripartum period [6]. Forty-five percent of all cases had no cause identified, highlighting that many cases of SCAD remain unexplained [4]. The commonest identified predisposing factors were postpartum, fibromuscular dysplasia (FMD), connective tissue disease and hormonal therapy [4]. Potential stressors include vigorous physical exertion particularly in young male patients, as it was the patient in our case, intense emotional stress, sympathomimetic drugs (such as cocaine, amphetamines), child-birth and Valsalva-like activities (such as coughing, retching, vomiting) [7]. Triggers for SCAD are thought to increase shear stress on the coronary artery wall, often mediated by elevated catecholamine levels and intra-abdominal pressure [8]. It is routinely advised to these patients to avoid intense isometric exercise (weight lifting as the patient in our case), competitive sports and emotional stress [9].
Type I dissection, which our patient had in the presented case, is the classic description of a longitudinal filling defect, representing the radiolucent intimal flap. There is often contrast staining of the arterial wall with a presentation of a double lumen [10].
Prognosis is favorable since our patient was stable. The risk for future events is minor, therefore patients should be advised of the risk of SCAD relapse. There is no effective treatment for prevention. An interesting observation is that in future relapses the affected vessels are different from them in the initial incident [11].
The time of achieving spontaneous healing varies according to different series where repeated CA was performed. It has been shown [4] that healing occurred >20 days after the dissection, a finding consistent with our case where spontaneous healing was late and was achieved after 6 months. Coronary CTA is a reasonable method to diagnose and follow cases with coronary dissections. However, it presents some limitations as it is rather unsuitable for type II or III dissections [12]. In addition, we had decided to perform an interventional method to follow the patient in order to diagnose exactly the time he could be healed.
Conservative management is preferred in stable patients with SCAD as most dissected segments will heal spontaneously [5]. Medical therapy is based upon opinion, with no randomized clinical trials in this area. Initial treatment is similar to standard ACS patients with the use of dual antiplatelet agents, heparin and beta-blockers to preserve the patency of the true lumen and prevent thrombotic occlusion. The duration of pharmacologic treatment is life-long, except for antiplatelet regimen since that clopidogrel could be discontinued at the end of one year. Many authors recommend this regimen, independently of the use of a coronary stent [12]. Glycoprotein IIb/IIIa inhibitors have also been used without complications. However, these agents could potentially delay the healing of the intramural hematoma and lead to dissection extension. Thrombolytic agents should not be used due to an increased risk of bleeding and extension of intramural hematoma [13]. It is known that statins are not routinely recommended in all cases with SCAD with the exception of specific indications [14]. However, the patient had hyperlipidemia. Besides, the finding of a single study that statin use was associated with higher risks of SCAD recurrence was not replicated in larger studies [12].
Conclusion
SCAD should be considered among the differential diagnosis in patients presenting with ACS, especially in particular situations (women, peripartum period, physical and emotional stress). When a spontaneous coronary dissection is observed, without any sign of ischemia, a follow-up is recommended with a conservative strategy to spontaneous healing. Studies or intensive observations are needed to establish a diagnosis and management strategy. Nature takes care of the rest.
Conflict of interest disclosure
None to declare.
Declaration of funding sources
None to declare.
Author contributions
Ioannis Vogiatzis: design, analysis and interpretation, drafting the article, final approval of the version; Konstantinos Koutsambasopoulos: conception and design, drafting the article; Pavlos Roditis: interventions, acquisition of data, images.
References
1. Rashid HN, Wong DT, Wijesekera H, Gutman SJ, Shanmugam VB, Gulati R, et al. Incidence and characterization of spontaneous coronary artery dissection as a cause of acute coronary syndrome. A single-centre Australian experience. Int J Cardiol. 2016;202:336-8.
2. Saw J, Mancini GBJ, Humphries KH. Contemporary Review on Spontaneous Coronary Artery Dissection. J Am Coll Cardiol. 2016;68(3):297-312.
3. Poon K, Bell B, Raffel OC, Walters DL, Jang IK. Spontaneous coronary artery dissection: utility of intravascular ultrasound and optical coherence tomography during percutaneous coronary intervention. Circ Cardiovasc Interv. 2011;4(2):e5-e7.
4. Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, Ricci D, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv. 2014;7(5): 645-55.
5. Yamauchi A, Nakagawa N, Shibayama K, Hirai T, Suzuki T, Kitaoka T, et al. Complete healing of spontaneous coronary artery dissection extending from the left main trunk to the left anterior descending and the left circumflex artery. J Cardiol Cases. 2018;18(3):103-5.
6. Garcia NA, Khan AN, Boppana RC, Smith HL. Spontaneous coronary artery dissection: a case series and literature review. J Community Hosp Intern Med Perspect. 2014; 4(4).
7. Nienaber CA, Powell JT. Management of acute aortic syndromes. Eur Heart J. 2012;33(1):26-35b.
8. Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J 2014;35(41):2873-926.
9. Chou AY, Prakash R, Rajala J, Birnie T, Isserow S, Taylor CM, et al. The First Dedicated Cardiac Rehabilitation Program for Patients with Spontaneous Coronary Artery Dissection: Description and Initial Results. Can J Cardiol. 2016;32(4):554-60.
10. Alfonso F, Bastante T, Cuesta J, Rodríguez D, Benedicto A, Rivero F. Spontaneous coronary artery dissection: novel insights on diagnosis and management. Cardiovasc Diagn Ther. 2015;5(2):133-40.
11. Saw J, Humphries K, Aymong E, Sedlak T, Prakash R, Starovoytov A, et al. Spontaneous Coronary Artery Dissection: Clinical Outcomes and Risk of Recurrence. J Am Coll Cardiol. 2017;70(9):1148-58.
12. Ingrassia J, Diver D, Vashist A. Update in Spontaneous Coronary Artery Dissection. J Clin Med. 2018;7(9):228.
13. Buccheri D, Piraino D, Cortese B. Spontaneous coronary artery dissection: A hint into its diagnosis and therapy. Int J Cardiol. 2016;215:545-7.
14. Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, Lennon RJ, et al. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation 2012; 126(5): 579-88.