ACHAIKI IATRIKI | 2020; 39(2):107–111
Case Report
Maria Lagadinou1, Ourania Kyriakopoulou1, Anastasia Karela1, Aggeliki Tsintoni2, Ioanna Stavroula Giannakopoulou2, Despoina Spyropoulou3, Dimitrios Velissaris2
1Emergency Department, University Hospital of Patras, Greece
2Internal Medicine Department, University Hospital of Patras, Greece
3Radiotherapy Oncology Department, University Hospital of Patras, Greece
Received: 12 March 2020; Accepted: 29 June 2020
Corresponding author: Maria Lagadinou, MD, PhD, Emergency Department, University Hospital of Patras, Greece, E-mail: m_lagad2004@yahoo.gr, mobile tel: +306983742532, tel: +302610999955
Key words: Hepatitis A, liver failure, liver transplantation, jaundice, renal impairment
Abstract
Hepatitis A is a disease, highly endemic in low-income countries and is associated with unsafe water or food, inadequate sanitation, poor personal hygiene and oral-anal sex. Epidemics related to contaminated food or water, can spread at an explosive rate. High risk groups for acquiring hepatitis A virus (HAV) infection include travelers to developing countries, children in daycare centers, sewage workers, male homosexuals, intravenous drug users and people in institutions. We present a rare case of a 42-year-old man, with hepatitis A acute liver failure and multiple organ involvement who recovered without liver transplantation. Hepatitis A remains an important cause of hepatitis outbreak and occasionally leads to fatal outcome.
Introduction
Hepatitis A, a highly contagious liver infection caused by hepatitis A virus (HAV) has plagued mankind for centuries. As an acute disease, it is associated with significant morbidity and occasional mortality [1]. Disease incidence varies greatly among countries and it is highly endemic in low-income ones [2].
HAV is spread via the intestinal-oral route. It is acquired through interpersonal contact, contaminated food or water, inadequate sanitation, poor personal hygiene and oral-anal sex. Vertical transmission from mother to fetus and transmission from blood or blood products have rarely been described. No identifiable source is found in 42% of all cases [1-3].
Hepatitis A virus can cause liver disease that ranges from mild to severe illness, but does not cause chronic liver disease [4]. The risk of fulminant hepatitis is high in patients having an underlying chronic liver disease and are over 40 years old [1].
Here, we present a rare case of a patient with hepatitis A acute liver failure with concomitant multiple organ insufficiency, who recovered without liver transplantation.
Case presentation
A 42-year-old man, was admitted to the University Hospital of Patras, Western Greece because of fever, chills and nausea. No diarrhea, vomiting, dysuria or abdominal pain were mentioned. Τhe patient reported the consumption of shellfish in an Egyptian city, forty days before admission and was under paracetamol (1.5-2gr daily) treatment since the week before admission. Regarding his medical history, the patient was heterozygous for beta-thalassemia, and was not prescribed any medication. He was not an intravenous (IV) drug user, smoker or addicted to alcohol. The patient did not report any history of immunization for HAV.
On admission, the patient was hemodynamically stable (heart rate 76 bpm and blood pressure 142/71mmHg), with respiratory sufficiency (respiratory rate 14 breaths/min and arterial blood oxygen saturation 99% in room air). Body temperature was up to 38.2oC. Jaundice was noticed on the skin and conjunctivas. The abdomen was soft, but with localized tenderness in the right hypochondrium.
Initial laboratory tests revealed elevated levels of liver enzymes and bilirubin and prolonged INR. (Main patients’ laboratory tests during hospitalization are reported in Table 1). Serologic tests for hepatitis B, hepatitis C, Leptospira, Borrelia, Leishmania and HIV were negative. The patient was not tested for hepatitis E. However, the hepatitis A virus tests (anti- HAV IgM and anti-HAV IgG) were positive confirming the diagnosis of acute hepatitis A accompanied by the clinical finding of jaundice. The right hypochondrium ultrasound showed borderline liver dimensions (elongated lobe diameter=17.5cm), thickness of the gallbladder wall, edema and presence of sound-reflecting sedimentary contents in its lumen and a mild dilatation of the intrahepatic biliary vessels. Splenoportal doppler sonography revealed no abnormalities (fig. 1).
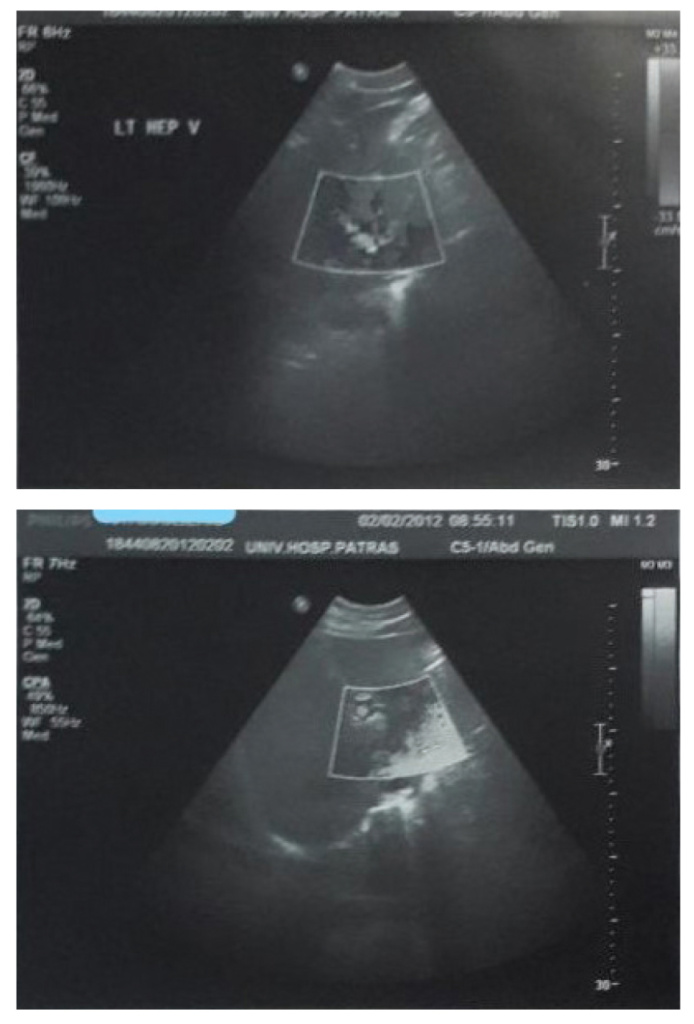
Figure 1. The ultrasound of right upper hypochondrium showed the liver with borderline dimensions, the gallbladder with thick wall, edema and presence of sound-reflecting sedimentary con-tents in its lumen.
The patient was admitted to the Internal Medicine Department under close monitoring and received IV fluids. He was also treated with N-acetylcysteine (1.5-2gr / day). Furthermore, four plasma units were administered aiming to restore coagulation abnormalities (to correct increased international normalized ratio-INR). After the 5th day of hospitalization, the patient’s level of consciousness was affected as he became lethargic with episodes of disorientation. Due to the severity of his condition he was immediately placed on the high-urgency waiting list for liver transplantation.
The deterioration of the patient’s level of consciousness was followed by severe complications including pneumonia, with fever relapse up to 38.3oC and moderate upper respiratory secretions (fig. 2). More specifically, there were radiological sings of lung infiltration in the lower right lung lobe with crackles on chest auscultation.
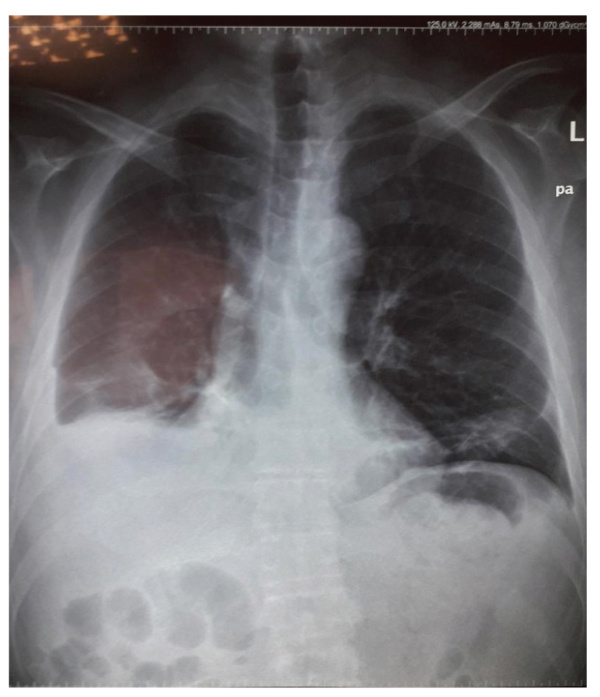
Figure 2. Chest X-ray showing radiological sings of pneumonia: lung infiltration and pleural effusion in lower right lung lobe.
At the same time (day 9 of hospitalization), renal dysfunction with elevated urea and creatinine and restricted urine output was detected. The patient was treated with meropenem [1 gr three times daily (td)] and vancomycin [500 mgr twice daily (bd)]. Blood and sputum cultures did not reveal any pathogen. The patient also received IV fluids and did not require continuous hemofiltration. Eventually, the patient showed a gradual and steady improvement in his clinical condition with a remarkable improvement of his consciousness level and an enhancement of his mental status as well as an improvement in laboratory parameters. On day 14 of hospitalization, the patient presented with not neurological deficit. His cardiovascular and respiratory status was stable, and renal function was restored to normal levels.
Discussion
Hepatitis A appears with multiple clinical manifestations. The most common signs and symptoms of the disease are fatigue, nausea and vomiting, abdominal pain or discomfort, especially on the upper right side of the abdomen, loss of appetite, fever, dark urine, joint pain, jaundice and intense itching. The symptoms may be relatively insignificant and disappear in a few weeks or severe, lasting for several months. Extra-hepatic manifestations, such as autoimmune hemolytic anemia, aplastic anemia, acute reactive arthritis, acute pancreatitis, mononeuritis and Guillain-Barré have also been reported [5-9].
Hepatitis A infection usually results in an acute, self-limiting illness conferring lifelong immunity and rarely leads to fulminant hepatic failure. In a Greek study among 286 patients admitted due to hepatitis A, 0.35% developed acute liver failure [2].This occurs more commonly in patients with an underlying liver disease (particularly chronic hepatitis B and C infection), advanced age or intravenous drug addiction [1].According to this, our case is a truly rare event during which a young patient experienced fulminant liver failure and encephalopathy without any predisposing factor.
In the rare case of fulminant hepatitis, patients should be early evaluated for possible liver transplantation. Orthotopic liver transplantation is the treatment of choice in patients with acute liver failure (ALF) who cannot recover with conservative treatment. Decision regarding liver transplantation should be individualized and based on the presence of clinical deterioration with sings of encephalopathy and decompensated liver function, as we did in the current case [10]. Oh SH et al, reported four cases of fulminant hepatitis A and acute renal failure, who underwent liver transplantation. In all cases, patients were older, were diagnosed with acute renal failure and showed hepatomegaly. Despite the severity of our patient’s disease, he improved without liver transplantation [11].
Jung DH et al reported 29 adult recipients, who underwent liver transplantation for HAV acute liver failure (ALF), at the Asan Medical Centre from January 2005 to December 2015 [3]. N-acetyl cysteine (NAC) has also been used in acute liver failure. It facilitates the synthesis of depleted glutathione, improves oxygenation by being used as a substrate for microsomal glutathione transferase and increases blood flow. It also demonstrates antioxidant and immunomodulatory properties [12]. In a study of 12 paediatric patients with ALF, it was reported that NAC appeared to be effective in ALF due to HAV, modifying the disease’s clinical course and preventing fatal outcomes. Similarly, in the present case, NAC treatment contributed to patient’s recovery. However, at present there is not adequate evidence regarding its use or the duration of its application [13].
In a nationwide multicentre study by Kwon SY et al, where 4,218 patients (mean age 33.3 yr) from 21 Korean tertiary centers were included, results showed that when symptomatic hepatitis A occurred, a significant number of patients experienced renal function impairment or prolonged cholestasis [14]. Renal insufficiency occurred in 2.7%, hepatic failure in 0.9%, relapsing hepatitis in 0.7%, and cholestatic hepatitis in 1.9% of patients. Nineteen patients (0.45%) died or were transplanted. The complications of renal failure and prolonged cholestasis were more frequent in patients older than 30 years [14]. A few cases of acute renal failure and nephrotic syndrome have been reported in the literature in association with hepatitis A infection. Acute tubular necrosis was the most common form of renal injury in these patients [1].
In the present rare case, the remarkable point is that the patient, despite having hepatic encephalopathy and being in a transplant waiting list, presented with a sudden improvement in his clinical condition and his laboratory results. The gradual and steady reduction of liver enzymes and bilirubin levels in combination with the improvement of consciousness level, led to general recovery. However, significant complications occurred including acute kidney insufficiency, respiratory infection and inconstant fever that prolonged the hospitalization period. Of great importance is the fact that the patient managed to avoid liver transplantation by receiving proper treatment for the chest infection, adequate hydration and plasma transfusion.
This is a rare case of a young patient at the age of 42 who experienced multiorgan dysfunction secondary to hepatitis A virus infection including fulminant liver failure, hepatic encephalopathy, acute renal failure and haematological dysfunction within a short time period and without any comorbidities or underlying liver disease.
Conflict of interest disclosure
None.
Declaration of funding sources
None.
Author contributions
Dimitrios Velissaris, Aggeliki Tsintoni: conception and design; Maria Lagadinou, Ioanna Stavroula Giannakopoulou, Ourania Kyriakopoulou, Anastasia Karela: interpretation of the data; Despoina Spyropoulou: drafting of the article; Maria Lagadinou: critical revision of the article for important intellectual content; Dimitrios Velissaris: final approval of the article.
References
1. Rasheed A, Saeed S. Acute hepatitis a virus infection presenting with multiorgan dysfunction: a case report. Cases J. 2009;2:8124.
2. Chi H, Haagsma EB, Riezebos-Brilman A, van den Berg AP, Metselaar HJ, de Knegt RJ. Hepatitis A related acute liver failure by consumption of contaminated food. J Clin Virol. 2014;61(3):456-8.
3. Jung DH, Hwang S, Lim YS, Kim KH, Ahn CS, Moon DB, et al. Outcome comparison of liver transplantation for Hepatitis A-related versus Hepatitis B-related acute liver failure in adult recipients. Clin Transplant. 2018;32(1).
4. Manka P, Verheyen J, Gerken G, Canbay A. Liver failure due to acute viral hepatitis (A-E). Visc Med. 2016;32(2):80-5.
5. Botero V, Garcia VH, Aristizabal AM, Gomez C, Perez P, Caicedo LA et al. Hepatitis A, cardiomyopathy, aplastic anemia, and acute liver failure: A devastating scenario. Transpl Infect Dis. 2018;20(2):e12842.
6. Hong SE, Choo JW, Lim SK, Lee SJ, Park JW, Kim SE, et al. A Case of Graves’ Disease Accompanied with Acute Hepatitis A Virus Infection. Korean J Gastroenterol. 2018;71(6):354-8.
7. Saito A, Saito M, Shimoe Y, Yoshimoto T, Kawakami M, Okamoto H, et al. Guillain-Barré syndrome associated with acute hepatitis A. A case report and literature review. Rinsho Shinkeigaku. 2018;58(9):574-7.
8. Mihori A, Nakayama M. Ataxic form of Guillain-Barré syndrome associated with acute hepatitis A. Gastroenterol Jpn. 1983;18(6):549-52.
9. Stübgen JP. Neuromuscular complications of hepatitis A virus infection and vaccines. J Neurol Sci. 2011;300(1-2):2-8.
10. Adhami T, Hannouneh I, Hepatitis A. Cleveland Clinic Center for Continuing Education: Disease Management. Feb, 2014.
11. Oh SH, Lee JH, Hwang JW, Kim HY, Lee CH, Gwak GY, et al. Four patients with Hepatis A presenting with fulminant hepatitis and acute failure who underwent liver transplantation, Korean J Hepatol. 2009 Sep;15(3):362-9.
12. Gunduz H, Karabay O, Tamer A, Özaras A, Mert A, Tabak OF. N-acetyl cysteine therapy in acute viral hepatitis, World J Gastroenterol. 2003;9(12):2698-700.
13. Muñoz-Martíneza SG, Díaz-Hernández HA, Suarez-Flores D, Sanchez-Avila JF, Gamboa-Dominguez A, García-Juárez I, et al. Atypical manifestations of hepatitis A virus infection. Revista de Gastroenterología de México (English Edition), 83(2), 134-43.
14. Kwon SY, Park SH, Yeon JE, Jeong SH, Kwon OS, Lee JW, et al. Clinical characteristics and outcomes of acute hepatitis a in Korea: a nationwide multicenter study. J Korean Med Sci. 2014;29(2):248-53.