ACHAIKI IATRIKI | 2022; 41(1):33–39
Review
Konstantina Kitsou1, Antonios Georgopoulos2, Theodora Katsila3, Dimitrios Kardamakis4
1School of Health Sciences University of Patras, Patras, Greece
2Department of Business Administration, University of Patras, Patras, Greece
3Institute of Chemical Biology, National Hellenic Research Foundation, Athens, Greece
4Department of Radiation Oncology, Department of Medicine, School of Health Sciences University of Patras, Patras, Greece
Received: 20 Aug 2021; Accepted: 28 Dec 2021
Corresponding author: D. Kardamakis, Department of Radiation Oncology, University of Patras Medical School, Patras, Greece, E-mail: kardim@upatras.gr
Key words: COVID-19, health crisis, radiotherapy, management
Abstract
The current COVID-19 pandemic has incited us to investigate the possibility of applying managerial changes to effectively deal with this health crisis within a Radiation Oncology Department in Greece.
We performed a literature review using the MEDLINE and PubMed databases up to July 2021, identifying the most relevant papers containing the keywords “COVID-19”, “management crisis” and “leadership”. We also analyzed the number of cancer patients referred for treatment to our Hospital and to our Department during the years 2019, 2020 and during the first quarter of 2021.
We propose a four-level plan of action to effectively manage this crisis, based on data derived from management theories and leadership. There was not a statistical difference in the number of patients referred and treated between years 2019 and 2020, as the measures taken did not affect the daily practice of the Department.
The COVID-19 pandemic has offered us the opportunity to review working practices and to realize that proper planning and prioritization of needs are important factors for the ordinary exercise of medicine. It revealed the potential of remote consultations in the context of telemedicine which, after careful assessment of its potential, could be considered as the modern revolution in medicine.
Introduction
The COVID-19 pandemic poses an enormous challenge not only for the Health Sector worldwide, but also for societies and national economies across the globe. This pandemic caused a crisis, which urged all Health Systems to abandon conventional practices and cope with the prevention of this infectious disease, its treatment, and the rehabilitation of infected patients, by utilizing all available resources. This health crisis is exaggerated by the fact that it is presently difficult to predict its duration. Many researchers have issued guidelines for the management of patients with COVID-19, focusing mainly or exclusively on the medical treatment of these patients in the hospital environment.
The word “crisis” originates etymologically from the Greek word “κρίσις (krisis)”, which means judgement, choice, or decision [1]. The use of the term, however, varies depending on the context in which it is being used and the researcher’s discipline [2].
When we refer to health crisis management, we imply that a coordinated and effective operational action plan of certain groups of people exists and is implemented in case of imposed threat to civilians’ health and health systems, regardless of cause and extent [3]. As a matter of fact, very few publications are dealing with management challenges caused by this crisis, in terms of management perspective, whilst, alarmingly, two recent publications assert that Health Systems have been wholly unprepared for this crisis [4,5].
This health crisis constitutes a challenge for any kind of health unit and especially for Radiotherapy ones, due to the peculiarities surrounding the treatment of oncology patients. The main concerns are mitigating the pandemic effects and ensuring the smooth provision of services.
The keys to success in a management crisis are good preparation, flexibility, having accurate data and demonstrating willingness to establish and implement the right measures by all the members of the department [6].
Consolidation management essentially includes all the measures and administrative policies that are chosen to be implemented for the organization to recover and return to a normal course. The consolidation manager must possess certain qualities, according to Hess et al. The most crucial ones are thinking in a systematic way and being willing to deal with any situation at hand [7]. This crisis has the characteristics of a life-threatening change to human environment, a high degree of uncertainty and the need for critical and potentially irreversible decisions [8]. Each of these phases differs in its content, duration, and management opportunities.
This study’s aim is to review all available literature on the management of the COVID-19 pandemic as a crisis, focusing on management guidelines. Then, based on these guidelines, the aim is to describe the actions taken in a small-sized Radiation Oncology Department within a tertiary public Hospital.
Materials and Methods
A comprehensive search of the MEDLINE and PubMed databases was undertaken for the period December 2019 until July 2021, with the following terms: COVID-19 AND management crisis (6 articles) /AND radiation oncology (912 articles) OR radiotherapy (613 results) / AND leadership (1101 articles), along with guidelines on COVID-19 and radiotherapy published by the ESTRO and ASTRO Societies (www.astro.org, www.estro.org).
A total of 2 articles were found to fit the search COVID-19 AND management crisis AND radiation oncology AND leadership [9,10].
We analyzed the number of new patients treated in our Department for every month, for the calendar years 2019, 2020 and the first quarter of 2021. We also calculated all new referrals to the Department and the number of patients diagnosed with cancer in our Hospital for the years 2019 and 2020.
Results
Based on available literature, we propose a “four level” action plan set to assist the doctor in acting under the capacity of a health crisis manager. The ways to address the current crisis can be included in this “four level” action plan and the proposed pandemic mitigation measures have been implemented in the Unit since March 2020 (Table 1).
Analysis of our data revealed that the average number of patients treated per month for the year 2019 was 55.6 ± 7.8, for the year 2020 52 ± 12.7 and for the first four months of 2021 it was 59.25 ± 11.18. The variables were examined for regularity by Kolmogorov-Smirnov and Shapiro-Wilk tests and it was found that they follow a normal distribution. Data processing does not show a statistically significant correlation between the years 2019 and 2020 (p = 0.189), although during the first lockdown imposed in Greece between March and May 2020, we observed a temporary decrease in the number of patients receiving radiotherapy. More precisely, this number was decreased by 22.4% for March, 39.1% for April and 31.4% for May. The Radiation Oncology Department accepted 676 new patients in 2019, while in 2020 this number was reduced by 4%, i.e., 648 new patients. The number of new patients with solid tumors and hematological malignancies who were diagnosed and / or treated at the University Hospital of Patras was 2773 for the year 2019 and 2519 for the year 2020, i.e., a decrease of 9.15% (Diagram 1).
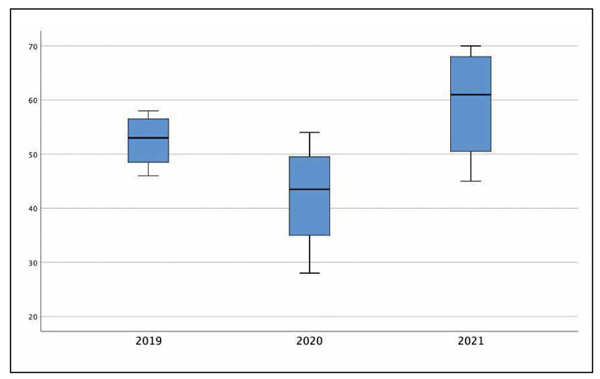
Diagram 1. Statistical data from the Radiation Oncology Department for the years 2019, 2020 and first quarter of 2021. Number of patients treated monthly.
Discussion
Regarding the workflow of Radiation Oncology Departments during the COVID-19 crisis, all accessible literature focuses on two main topics:
Generally applied medical guidelines
A basic priority is the prevention or mitigation of transmission forms among patients with cancer and the personnel. The guidelines produced by various Societies are presented in the publication of Mauri et al. [11].
Measures specific to Radiation Oncology Departments
Dinh et al. present specific guidelines applied in Radiation Oncology Departments regarding not only the mitigation of disease transmission, but also the applied practices in the Department in terms of patient treatment and care [12]. In a paper published by Hinduja et al. from India, the finer details associated with running a Radiation Oncology department in times of a pandemic are presented [13].
But the key issue for Radiation Oncology Department remains treatment priority that should be given to cancer patients according to the site and stage of the disease. Pandemics like the one caused by COVID-19 raise not only medical questions which cannot always answered by the data from evidence-based oncology, but also ethical dilemmas because of limited resources and increased risks of infection. Simcock et al. presented a simple model for the harm associated with COVID-19 infection in cancer patients [14]. They concluded that although colleagues around the world have dealt with enormous service pressures in the face of natural disaster or infections previously, the global scale and challenge of COVID-19 is unprecedented. For radiation oncology, this includes best practices from frameworks used successfully in other crises, published evidence, and international input. In line with previous recommendations, we urge units to proactively prepare their departments with training and Personal Protection Equipment and evaluate their infection control procedures. Departmental agreements on adapting remote working practices and hypofractionation regimes (or even avoiding or delaying treatment) are likely to reduce the burden of this disease on our cancer population. It is worth to mention here that the delay in offering radical or adjuvant radiotherapy, is associated with increased mortality for breast, head and neck and cervix cancer patients [15]. The use of social media has proven a very effective method of colleagues globally networking and sharing insight and experience.
COVID-19 as a management crisis in a Radiation Oncology Department
The term “crisis” is characterized as “high consequence, low probability, overlaid with risk and uncertainty conducted under time-pressure, disruptive of normal business and potentially lethal to organizational reputation”, according to Ann Gregory [16]. Additionally, by way of definition, “public health crisis” is a sequence of events affecting humans in one or more geographic areas, following a public health threat, with limited time available for deciding and a large degree of uncertainty leading to the limitation of normal response capacity. Health crises generally have significant impacts on community health, loss of life, and on the economy. Its severity is often measured by the number of people affected, by its geographical extent, or death rate of the pathogenic process from which it originates. Synonym to that is “public health emergency”, which according to WHO [17] is defined as “an occurrence or imminent threat of an illness or health condition, caused by bio terrorism, epidemic or pandemic disease, or (a) novel and highly fatal infectious agent or biological toxin, that poses a substantial risk of a significant number of human facilities or incidents or permanent or long-term disability”.
Historically, humanity has experienced several pandemics caused by infectious agents in the last 100 years: The Spanish flu in 1918, the HIV/AIDS in 1981 till today, the “Swine flu” or H1N1/09 pandemic in 2009 and the recent SARS-CoV epidemic.
In their publication Begun and Jiang introduce the concept of “Complexity Science”, which views health care delivery organizations as complex adaptive systems that operate in highly complex and unpredictable environments. They concluded that Complexity Science puts emphasis on simple rules, open discussions and building connections and provides an orienting framework for response to major surprise [18].

Figure 1. Illustrative presentation of the COVID-19 crisis.
Ways to address the current crisis (pandemic), to overcome the obstacles on patient’s health and disease prognosis can be summarized in the following plan of action (Figure 1, Table 1):
- Mobilization (Mobilize): According to Watkins and Bazerman, the rationale for dealing with a crisis is to identify the emerging threat in a timely manner, prioritize it and mobilize it quickly by means of effective measures [19]. At this stage the aim is to react and adapt quickly to the new data.
- Stabilization of the new situation (Stabilize): The affected Organization is now faced with a crisis, but with the proper preparation and implementation of the appropriate measures taken, it succeeds in stabilizing itself in this new situation and then, after a “x” period, it can achieve a gradual return to normality. The aim at this stage is to establish and strengthen the measures and practices introduced in the “Mobilization” phase.
- Strategy (Strategize): During a crisis, the new environment is deemed unstable and highly changing, and the personnel is operating under tension, as well as pressure, but also uncertainty due to a lack of a clear perspective on the outcome. At this point, the implementation of a sound strategy is the most important tool for assessing the measures taken. The overall strategic objectives, which must be measurable and realistic, the identification of strengths and weaknesses of the organization as well as opportunities for threats from the external environment, as well as the overall action plan, are part of a coherent and operational-strategic planning [20]. The goal at this level was to redesign and develop an operational strategy for a successful transition to normalization.
- Anti-aliasing (Re-normalize): The final phase of the crisis cycle in an Organization is normalization [21]. The objective of this step is the gradual return to normality, which is currently not visible.
The analysis herein will allow us to perceive this pandemic in terms of management and leadership and will help us to delimit the crisis in a more general content, whilst, simultaneously, measure more accurately the economic repercussions for the Health Sector. And most important, this analysis will assist Organizations in designing and establishing a “crisis-sensitive plan” with the support of health-policy makers.
The COVID-19 pandemic has currently gone into a catastrophic new chapter according to Johns Hopkins statistics (22). So far, a total of 245.092.869 people has been infected, while 4.973.610 have died (27 October 2021). Compared with COVID-19, the earlier epidemic of SARS and MERS was much slower in spreading around the globe. Increased globalization, international traveling, and virus adaptability in almost all countries without distinction are often reported as the primary reasons behind the rapid spread. The latter is also attributed to the risk assessment regarding COVID-19 virulence capacity. To date, there is no single specific therapeutic option for battling against this virus.
Considering the recent findings by Bardet et al. from France, diagnostic and treatment delays in patients with cancer, due to COVID-19, may have an impact on patient physical and mental health and on survival per se [23]. These delays, rescheduled or cancellation in radiotherapy, have been one of the main problems that oncological patients have faced. Due to the same reason, the post-treatment follow-up programs have also been affected. Consequently, to tackle the post lock down patient backlog, we have extended working hours in the Department and we continue to prioritize patients according to the diagnosis [24].
This crisis revealed the potential of remote consultations in the context of telemedicine which, after careful assessment of its potential, could be considered as the modern revolution in medicine. Telemedicine (telehealth) can provide remote support to patients thereby reducing physical access to the hospitals and costs [25,26]. Along with this technology facilitation comes Artificial Intelligence-based imaging analysis and health informatics for monitoring patients [27].
Telemedicine can be of great help in the management of patients who recovered from the infection but need rehabilitation. Salawu et al propose a model of tele-rehabilitation as an alternative to traditional face-to-face intervention [28].
It appears that almost twenty-two months after the start of the pandemic the operating system of the Radiation Oncology Department is in a stabilization phase and the effectiveness of all measures is becoming apparent. The time frame until full recovery to normality is certainly unknown at present and depends on four main variables: (a) the effectiveness of measures to reduce the spread of the virus, and in particular the vaccination program, (b) the effectiveness of budgetary and economic measures, (c) the ability of the health system to maintain and increase its ability to handle the volume of critically-ill patients, and (d) the timing of the availability of specialized medicinal products for the treatment of the disease. This study was conducted in one, medium-sized by Greek standards, Radiation Oncology Department and it is based on home statistics and relevant literature. In other words, the proposed plan of action is based on existing literature data and not on data accumulated during the crisis. We are planning to form a properly structured questionnaire among the personnel working in Radiation Oncology Departments at a national level, to identify the appropriate measures and practices adopted during a health crisis. Additionally, although all information included in this study must be interpreted in the context of the current COVID-19 situation, it can be of a great assistance for resolving future health crisis caused by a natural disaster, terrorism, or a new pandemic. It is important to organize in the Department a “Network of Teams” which can serve common purposes such as workforce protection, operation of the treatment machines (linear accelerators) and prompt communication with patients and their caregivers.
Conclusions
This pandemic has presented us with challenges that we have not been exposed to so far. For the personnel of Radiation Oncology Departments, the rule “Do not cancel treatments” has been applied. This crisis strengthened the group’s links and redefined the concepts of collective and individual responsibility. It has granted us the opportunity to review working practices and realize that proper planning and prioritization of needs are important factors for the safe exercise of medicine.
An important parameter in everyday practice was the introduction of telemedicine, aiming at reducing the exposure of patients and staff by face-to-face appointments. Although this adjustment under COVID-19 will continue, we must be reluctant to move to its routine use without careful patient selection. We must consider multiple parameters ensuring that we maintain effective and safe healthcare to our patients.
Strong leadership, quality communication and clear direction are required during this crisis to ensure that radiation therapists receive all necessary support and resources required to maintain their safety and patient’s well-being during the COVID-19 pandemic.
Conflict of interest disclosure
None to declare
Declaration of funding sources
None to declare
Author contributions
K. Kitsou: collection – analysis – interpretation of data, drafting of the article, final approval of the article; A. Georgopoulos: collection – analysis – interpretation of data, drafting of the article, final approval of the article; T. Katsila: collection – analysis – interpretation of data, drafting of the article, final approval of the article; D. Kardamakis: study design, drafting of the article, final approval of the article.
References
1. Paraskevas A. Crisis management or crisis response system?: A complexity science approach to organizational crises. Manag Decis. 2006;44(7):892–907.
2. Preble JF. Integrating the crisis management perspective into the strategic management process. Vol. 34, Journal of Management Studies. Blackwell Publishing Ltd; 1997. p. 768–91. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/1467-6486.00071
3. Efstathiou P, Papafragkaki D, Gogosis K, Manwlidou Zacharoula. Crisis Management in the Health Sector: Qualities and characteristics of health crisis managers. Int J Caring Sci. 2009;2(3):105–7.
4. Horton R. Offline: COVID-19 and the NHS—“a national scandal” . Lancet. 2020;395(10229):1022.
5. Gallina P, Ricci M. Covid-19 health crisis management in Europe: Decisive assessment is needed now. Int J Infect Dis. 2020; 96: 416.
6. Butler M, Rivera K. How to respond when a crisis becomes the new normal. 2020. Available from: https://www.strategy-business.com/blog/How-to-respond-when-a-crisis-becomes-the-new-normal?gko=ff6a3
7. Hess H, Fechner D, Feund K, Körner F. Sanierungshandbuch. Berlin:Luchterhand: Kriftel; 1998.
8. Thomas C. Coping with Crises: The Management of Disasters, Riots and Terrorism. Rosenthal, Uriel; Charles MT., and ’t Hart P, editors. Vol. 16, Australian Journal of Management. Springfield; 1989. p. 99–102.
9. Jazieh AR, Chan SL, Curigliano G, Dickson N, Eaton V, Garcia-Foncillas J, et al. Delivering Cancer Care During the COVID-19 Pandemic: Recommendations and Lessons Learned From ASCO Global Webinars. JCO Glob Oncol. 2020;(6):1461–71.
10. Rossi B, Zoccali C, Baldi J, Scotto di Uccio A, Biagini R, De Luca A, et al. Reorganization Tips from a Sarcoma Unit at Time of the COVID-19 Pandemic in Italy: Early Experience from a Regional Referral Oncologic Center. J Clin Med. 2020;9(6):1868.
11. Mauri D, Kamposioras K, Tolia M, Alongi F, Tzachanis D, collaborators IOP and ECPC. Summary of international recommendations in 23 languages for patients with cancer during the COVID-19 pandemic. Lancet Oncol. 2020;21(6):759–60.
12. Dinh TKT, Halasz LM, Ford E, Rengan R. Radiation Therapy in King County, Washington During the COVID-19 Pandemic: Balancing Patient Care, Transmission Mitigation, and Resident Training. Adv Radiat Oncol. 2020;5(4):544–7.
13. Hinduja RH, George K, Barthwal M, Pareek V. Radiation oncology in times of COVID-2019: A review article for those in the eye of the storm – An Indian perspective. Semin Oncol. 2020;47(5):315-27.
14. Simcock R, Thomas TV, Estes C, Filippi AR, Katz MA, Pereira IJ, et al. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68.
15. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020;371:m4087.
16. Gregory A. Communication dimensions of the UK foot and mouth disease crisis, 2001. J Public Aff. 2005;5(3–4):312–28.
17. Global action plan on the public health response to dementia [Internet]. [cited 2021 Apr 17]. Available from: http://apps.who.int/bookorders.
18. Begun JW, Jiang HJ. Characteristics of the Covid-19 Pandemic Health Care Management During Covid-19: Insights from Complexity Science. NEJM Catalyst. 2020.
19. Watkins MD, Bazerman MH. Predictable Surprises: The Disasters You Should Have Seen Coming. Vol. 81, Harvard Business Review. 2003. Available from: https://www.hbs.edu/faculty/Pages/item.aspx?num=14330
20. Van Wijngaarden JDH, Scholten GRM, Van Wijk KP. Strategic analysis for health care organizations: The suitability of the SWOT-analysis. Int J Health Plann Manage. 2012;27(1):34–49.
21. Valackiene A, Virbickaite R. Conceptualization of crisis situation in a company. J Bus Econ Manag. 2011;12(2):317–31.
22. Hopkins J. COVID-19 Map – Johns Hopkins Coronavirus Resource Center. Johns Hopkins Coronavirus Resource Center. 2020. p. 1. Available from: https://coronavirus.jhu.edu/map.html
23. Bardet A, Fraslin AM, Marghadi J, Borget I, Faron M, Honoré C, et al. Impact of COVID-19 on healthcare organisation and cancer outcomes. Eur J Cancer. 2021;153:123–32.
24. Osei E, Francis R, Mohamed A, Sheraz L, Soltani-Mayvan F. Impact of COVID-19 pandemic on the oncologic care continuum: urgent need to restore patients care to pre-COVID-19 era. J Radiother Pract. 2021:1–11.
25. Zon RT, Kennedy EB, Adelson K, Blau S, Dickson N, Gill D, et al. Telehealth in Oncology: ASCO Standards and Practice Recommendations. JCO Oncol Pract. 2021;17(9):546-64.
26. Al‐Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 ( COVID ‐19) Pandemic: An International Collaborative Group . Oncologist. 2020;25(6).
27. Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6(6):CD000072.
28. Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A Proposal for Multidisciplinary Tele-Rehabilitation in the Assessment and Rehabilitation of COVID-19 Survivors. Int J Environ Res Public Health. 2020;17(13):4890.