ACHAIKI IATRIKI | 2021; 40(1):44–48
Original research article
Aikaterini Solomou1, Pantelis Kraniotis1, Nikolaos Ntoulias2, Anastasios Apostolos2, Irene Tsota3, Aspasia Rigopoulou1
1MR Department, University General Hospital of Patras, Patras, Greece
2Department of Medicine, University of Patras, Patras, Greece
3Ultrasound Department, General Hospital of Patras, Patras, Greece
Received: 11 Oct 2020; Accepted: 27 Jan 2021
Corresponding author: Aikaterini Solomou, Professor of Radiology-MRI, Head og MRI Department of MR Department, Faculty of Medicine, Department of Radiology, University Hospital of Patras, 265 04, Rio- Patras, Greece, Tel.: +30 2613 603422, E-mail: solomou@med.upatras.gr
Key words: Renal abscess, ultrasonography, magnetic resonance imaging, diffusion weighted imaging, pyelonephritis, women’s health
Abstract
Background: Renal abscess is a rare complication of acute pyelonephritis. Radiologic imaging is important, bearing in mind the lack of laboratory tests’ specificity for the diagnosis of an abscess. It mostly occurs in diabetes mellitus patients (75% of abscesses) and/or in the existence of a stone, with young women being the most affected population. Our goal was to highlight the optimal imaging protocol, in the work-up of complicated pyelonephritis in young women, trying to avoid radiation exposure.
Methods: Four (4) cases of renal abscess following acute pyelonephritis in women of relatively young age, ranging from 17 to 22, who were admitted to our hospital in a 18-months period. All patients were submitted to ultrasound (U/S) examination and one patient to Magnetic Resonance Imaging (MRI).
Results & Conclusions: Because of its availability and low cost, U/S appears to be the first-line imaging technique for the investigation of a renal abscess after acute pyelonephritis. Particularly in cases of young women where imaging findings or laboratory tests are inconclusive, MRI with diffusion-weighted images (when available) should be used as an adjunct to confirm the abscess, obviating the need of radiation exposure.
Introduction
Pyelonephritis is one of the many faces of Urinary Tract Infection (UTI) and the formation of renal abscess is considered a rare clinical complication [1]. It mostly occurs in diabetes patients (75% of abscesses) and/or with coexisting renal calculi with young women being the most affected population [2]. Fortunately, the improvement of imaging techniques (Ultrasound (U/S), Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) in combination with the advancement of medical treatment and the wide application of interventional techniques, like percutaneous abscess drainage, have significantly decreased mortality rates from 40-50% to about 1.5%-15% in the last three decades [3].
We herein report a case series of renal abscesses in young women, highlighting the most prevalent imaging features and stressing-out the necessary imaging protocol, in order to avoid radiation exposure.
Materials and methods
We detected four cases of renal abscesses following acute pyelonephritis between May 2018 and November 2019 from our hospital archives. All patients were Caucasian women of young age, ranging from 17 to 24 years old, that were admitted to our hospital due to clinical manifestations resembling those of UTI and especially pyelonephritis. The right kidney was affected in 3 of the 4 cases. Patients did not present any other comorbidity, chronic medical treatment or had a history of a surgical procedure.
After a clinical examination and relevant laboratory tests, all patients were initially imaged with U/S scan [5]. In one case, with inconclusive clinical and lab tests, further imaging was needed. The patient was pregnant and could not be submitted to CT. In order to confirm the diagnosis, the latter patient was submitted to MRI, with DWI, without intravenous Gadolinium administration.
Results
U/S
Patients were scanned with a convex probe and both grayscale and color Doppler images were acquired. The location of the abscesses was mainly cortical. Largest dimensions ranged between 1.5 to 2.4cm. The lesions were mainly hypoechoic. On color Doppler there was no vascularity within the lesions, apart from one where there was minimal internal vascularity. All cases presented with a small amount of perirenal fluid. Renal calculus was detected in one case. Ultrasound findings are summarized in Table 1. Ultrasound imaging findings are highlighted in Fig. 1-4.
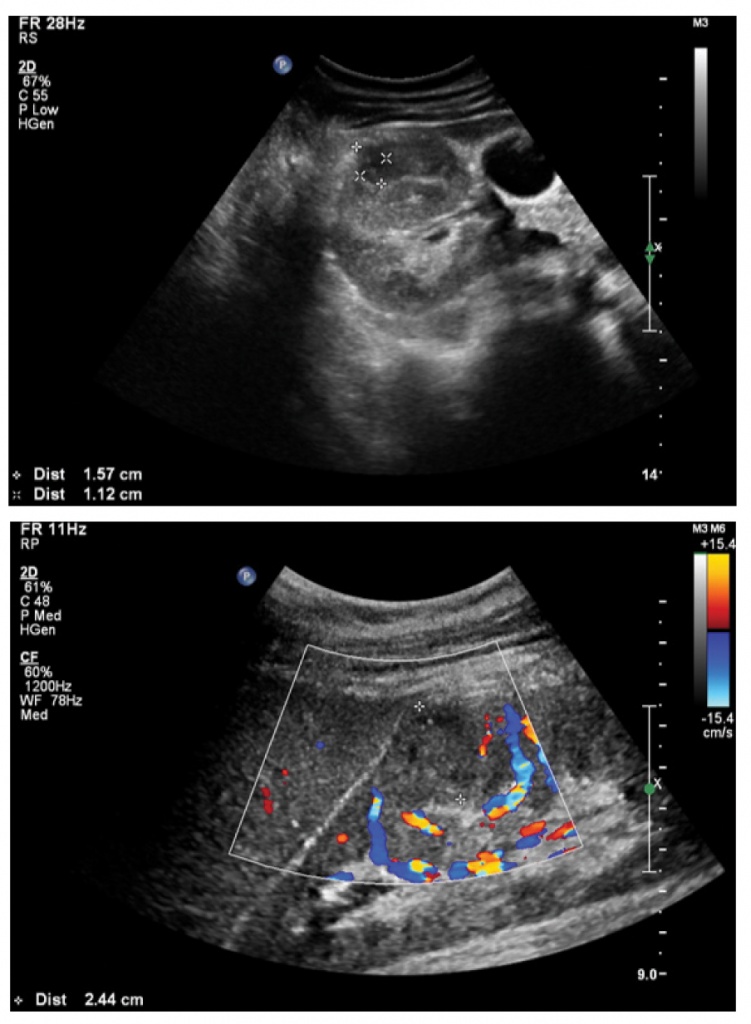
Figure 1 (a-b). Patient #1. Ultrasound images, grayscale (a) and color doppler (b) show a well-defined inhomogeneously hypoechoic lesion, (largest dimension 1.5cm) within the renal cortex which has a more hypoechoic center. On color Doppler the lesion is hypovascular with only peripheral vascularity (b).
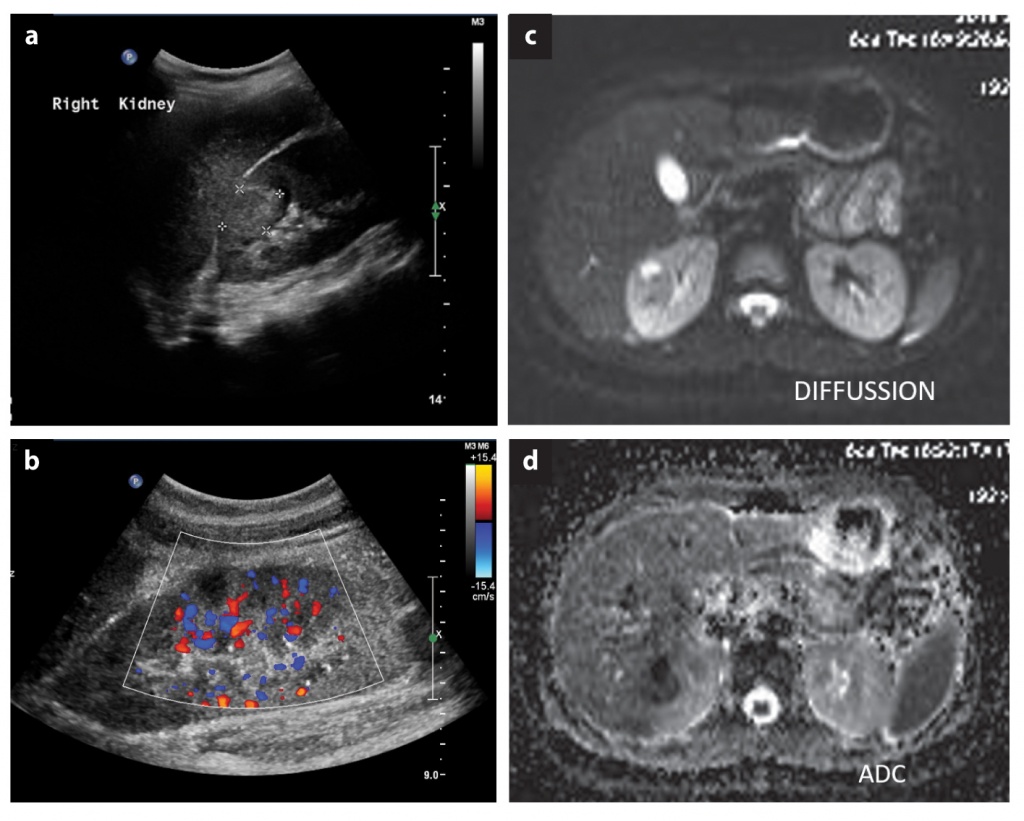
Figure 2 (a-b). Patient #2. Ultrasound images, grayscale (a) and color doppler (b) show a well-defined inhomogeneously hyperechoic lesion (largest dimension 1.5cm), within the renal cortex which has a more hypoechoic center. On color Doppler the lesion is hypovascular with peripheral vascularity only (b). (c-d). Patient #2. Axial DWI (c) and corresponding ADC map (d). The lesion is hyperintense on the DWI and hypointense on the ADC, consistent with true diffusion restriction.
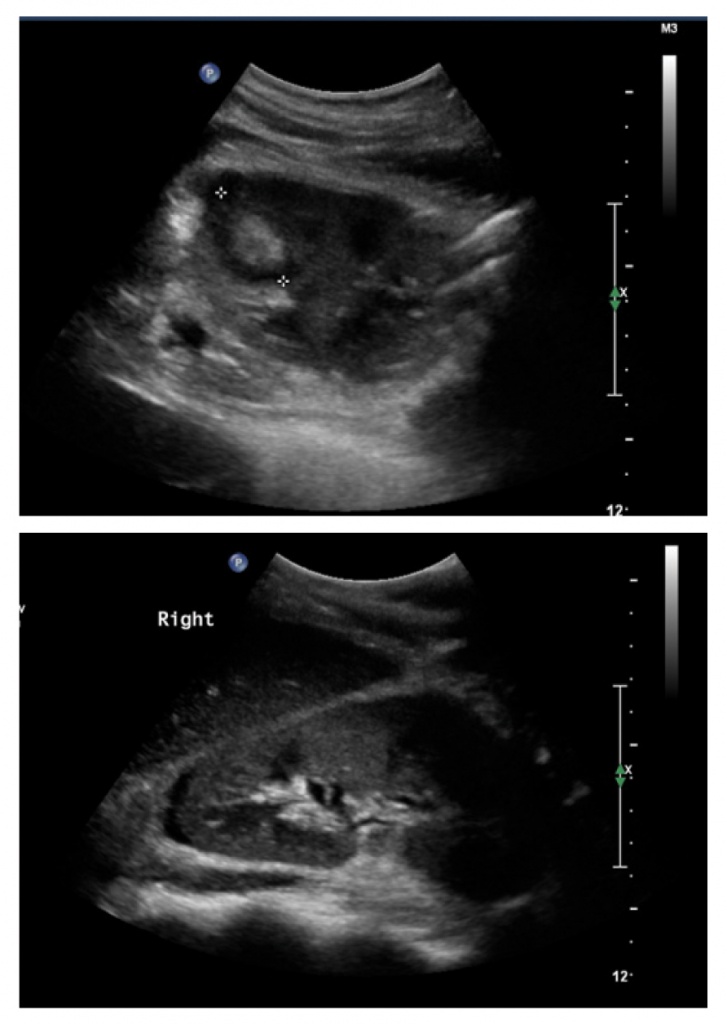
Figure 3 (a-b). Patient #3. Ultrasound grayscale images show a well-defined lesion within the renal cortex (largest diameter 1.6cm) with mixed echogenicity and predominantly hyperechoic center (a). There is also a small quantity of perirenal fluid around the upper pole of the kidney (b).
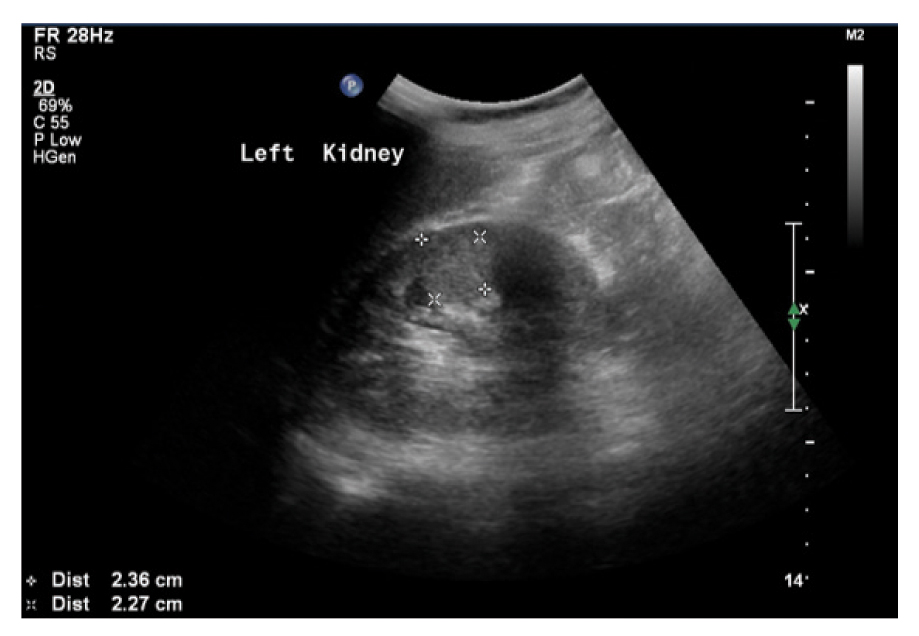
Figure 4. Patient #4. Α hyperechoic lesion (largest diameter 2.4cm) centered within the corticomedullary region.
MRI
The MRI protocol included T2WI TSE coronal and axial planes, T2WI TSE axial with fat- suppression images; Diffusion balances 0, 50, 100, 150, 500, T1 GRE with fat suppression axial and coronal images and T1WI GRE in- and opposed phase in the transverse plane. The abscess detected as an inhomogeneous lesion with internal moderately high T2-WI signal, surrounded by a thin hypointense wall. There was restricted diffusion with high signal in the DWI images and low values in the corresponding ADC map, in keeping with an abscess (Fig. 2c-d).
Discussion
Renal abscesses may occasionally be present in patients with pyelonephritis as a focal or hematogenous complication [6]. The main risk factors include: diabetes mellitus, renal calculi and ureteral obstruction. The clinical outcome of the patient relies mainly on early diagnosis, so radiological imaging plays a significant role [7]. Laboratory tests are not specific for the diagnosis of renal abscess; however, the diagnosis is established with U/S or CT/ MRI studies. U/S is the first line imaging modality performed because of its low cost, feasibility, widespread availability, and low examination time. However, CT with contrast agent outmatches US in the diagnosis of renal abscesses with a very high diagnostic rate [8]. CT finds great usage in cases of inconclusive U/S diagnoses, assessing accurate abscess size and extension and providing information about kidney function. Additionally, CT is important in the follow-up of medical treatments. On the other hand, despite the higher sensitivity and specificity of MRI and its overall diagnostic value, it is not used as a first line diagnostic technique, due to its relative inaccessibility and its higher cost. MRI is essential in patient’s follow-up imaging and in cases that require avoiding radiation dose such as paediatric patients or pregnant patients. However, all the above-mentioned techniques contribute to the earliest possible diagnosis, management and follow-up of patients with renal abscesses following acute pyelonephritis [9]. A renal abscess in the ultrasonography usually presents as a well- or moderate-defined hypoechoic lesion, rarely with internal hyperechogenicity. It is usually located in the cortex or in the cortico-medullary parenchyma, regularly accompanied by perinephric collection. Septations and loculations have been described into renal abscesses. The differential diagnosis between a renal abscess and focal nephritis remains an issue for radiologists; focal nephritis usually presents with smaller lesions with poorly defined borders. The combination of acute pyelonephritis is demonstrated by a hypoechoic kidney [10]. Studies using Doppler show absence of vascularity in the necrotic pus-filled region, while the flow in the wall may be variable. A modern approach includes contrast-enhanced U/S for evaluating renal abscesses, which provides better specificity and sensitivity comparing to classic U/S. In addition, it has been supported that contrast-enhanced may be equal to CT on imaging quality, while it can be applied even in young women avoiding radiation exposure [11]. On CT, early abscess emerges as ill-defined hypoattenuating non-enhancing lesion. In the contrary, late abscess appears as well-defined hypoattenuating lesion surrounded by a thick irregular enhancing/hypervascular wall. The presence of gas within a hypoattenuating cystic formation is compatible with an abscess. Unenhanced CT is useful to provide information about calculi, gas-forming infections, haemorrhage, and parenchymal calcifications, while the use of intravenous contrast material especially the nephrographic phase (50-90 seconds) is essential for the diagnosis of renal abscess due to the significant differentiation between the normal enhancing renal parenchyma and hypovascular lesions [12,13]. Computed tomography (CT) is considered the gold standard imaging modality not only for the diagnosis and assessment of acute pyelonephritis but also for the severity of inflammation and its complications such as an abscess. However, it should not be used in young women and especially during pregnancy, due to radiation exposure concerns. MR-imaging is essential for the diagnosis of abscesses although its usage is limited. The use of diffusion-weighted images provides immediate and accurate diagnosis as it shows restriction of diffusion with low signal of the affected area, in the ADC map, which is indicative of renal abscess. Contrary to CT, it can be used for further investigation of renal abscesses especially in children and young women where radiation protection concerns are raised. [12,14]
The specificity and sensitivity of the imaging methods are not well-established with important variance, as it is affected by physicians’ experience and abscess’ characteristics. It is supported that newer applications of US, like tissue harmonic imaging have reported sensitivity and specificity equivalent to 97% and 80%, respectively [15]. CT provides higher sensitivity and specificity (>90%) than US, when an intravenous agent is administered [16]. The existing literature do not analyze the prognostic value of MRI for renal abscesses as a diagnostic approach.
Conclusion
The formation of an abscess due to pyelonephritis is very uncommon. CT is considered the gold standard examination to detect renal abscess, when clinical concern is raised, according to the literature. However, in cases of very young women of child-bearing age and/or in cases of pregnant women ultrasound should be the first line investigation. In inconclusive cases, MRI with DWI (when available) should be used instead of CT in order to avoid radiation exposure in this sensitive group. Furthermore diffusion-weighted images can characterize the lesion without the need for IV Gadolinium administration.
Conflict of interest disclosure: None to declare.
Declaration of funding sources: None to declare.
Author contributions: AS and PK: conception and design of the work; acquisition, analysis and interpretation of data, drafting and revising the manuscript critically for important intellectual content, and final approval of the version to be published; NN, AA and AR: conception and design of the work; acquisition, analysis and interpretation of data, drafting and revising the manuscript critically for important intellectual content; IT: drafting and revising the manuscript critically for important intellectual content.
References
- Belyayeva M, Jeong JM. Acute Pyelonephritis. [Updated 2020 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519537/
- Craig W, Wagner B, Travis M. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28(1):255-77; quiz 327-8.
- Czaja CA, Scholes D, Hooton TM, Stamm WE. Population-based epidemiologic analysis of acute pyelonephritis. Clin Infect Dis. 2007; 45(3):273–280.
- Rubilotta E, Balzarro M, Lacola V, Sarti A, Porcaro AB, Artibani, W. Current Clinical Management of Renal and Perinephric Abscesses: A Literature Review. Urologia. 2014;81(3):144-147.
- Goel RH, Unnikrishnan R, Remer EM. Acute Urinary Tract Disorders. Radiol Clin North Am. 2015;53(6):1273–1292.
- Grabe M, Bjerklund-Johansen TE, Botto H, Çek M, Naber KG, Pickard RS. Guidelines on Urological Infections. European Association of Urology (EAU). 2013; 4.4.2;30-1.
- Sung BJ, Chung JM, Choi S, Rhew HY, Lee SD. Renal and Perinephric Abscesses: Ten Years of Experience at a Single Center. Korean J Urol. 2008; 49(10):923-30.
- Coelho RF, Schneider- Monteiro ED, Mesquita JL, Mazzucchi E,Marmo Lucon A, Srougi M. Renal and perinephric abscesses: Analysis of 65 consecutive cases. World J Surg. 2007;31(2):431-6.
- Enikeev DV, Glybochko P, Alyaev Y, Enikeev M, Rapoport L. Imaging Technologies in the Diagnosis and Treatment of Acute Pyelonephritis. Urologia. 2017;84(3):179–184.
- Kao H-W, Wu C-J. Ultrasound of Renal Infectious Diseases. J Med Ultrasound. 2008;16(2):113–122.
- Fontanilla T, Minaya J, Cortés C, Hernando CG, Arangüena RP, Arriaga J, et al. Acute complicated pyelonephritis: contrast-enhanced ultrasound. Abdom Imaging. 2012;37(4):639-646.
- Colgan R, Williams M, Johnson JR. Diagnosis and treatment of acute pyelonephritis in women. Am Fam Physician. 2011;84(5):519-526.
- Pallwein-Prettner L, Flöry D, Rotter CR, Pogner K, Syré G, Fellner C, et al. Assessment and characterisation of common renal masses with CT and MRI. Insights Imaging. 2011;2(5):543-556.
- Chen CY, Kuo HT, Chang YJ, Wu KH, Yang WC, Wu HP. Clinical assessment of children with renal abscesses presenting to the pediatric emergency department. BMC Pediatr. 2016;16(1):1–5.
- Lee SH, Jung HJ, Mah SY, Chung BH. Renal abscesses measuring 5 cm or less: outcome of medical treatment without therapeutic drainage. Yonsei Med J. 2010;51(4):569-573.
- Dalla Palma L, Pozzi-Mucelli F, Ene V. Medical treatment of renal and perirenal abscesses: CT evaluation. Clin Radiol. 1999;54(12):792-797.