ACHAIKI IATRIKI | 2025; 44(Suppl 1):18–20
Editorial
Nicholas G. Kounis1, Ioanna Koniari1, Virginia Mplani2
1Department of Medicine, Division of Cardiology, University of Patras Medical School, Patras, Greece
2Intensive Care Unit, Patras University Hospital, 26504 Patras, Greece
Received: 14 Sep 2025; Accepted: 29 Sep 2025
Corresponding author: Nicholas G. Kounis, Department of Medicine, Division of Cardiology, University of Patras Medical School, Patras, Greece, ngkounis@otenet.gr
Keywords: Anti-IgE, immunoglobulin E, coronary spasm, coronary thrombosis, Kounis syndrome, mast cells
Introduction
Currently, Kounis syndrome refers to coronary syndromes linked with mast cell-associated illnesses and inflammatory cell interactions, such as those involving T-lymphocytes and macrophages, which intensify allergic, hypersensitive, anaphylactic, or anaphylactoid shocks.
Interactions via multidirectional stimuli functioning as a “ball of thread,” post-inflammatory cell activation, and inflammatory mediators generated following an allergic assault are the causes of this illness [1]. Additionally participating in this process is a 20% platelet subgroup with IgE (immunoglobulin E) surface receptors of both high and low affinity.
Kounis Syndrome
Kounis syndrome is now recognized as a distinct form of acute vascular syndrome [2] that impacts the cerebral, mesenteric, peripheral arterial, and venous systems in addition to the coronary arteries, resulting in angina, infarction, and stent thrombosis (Figure 1).
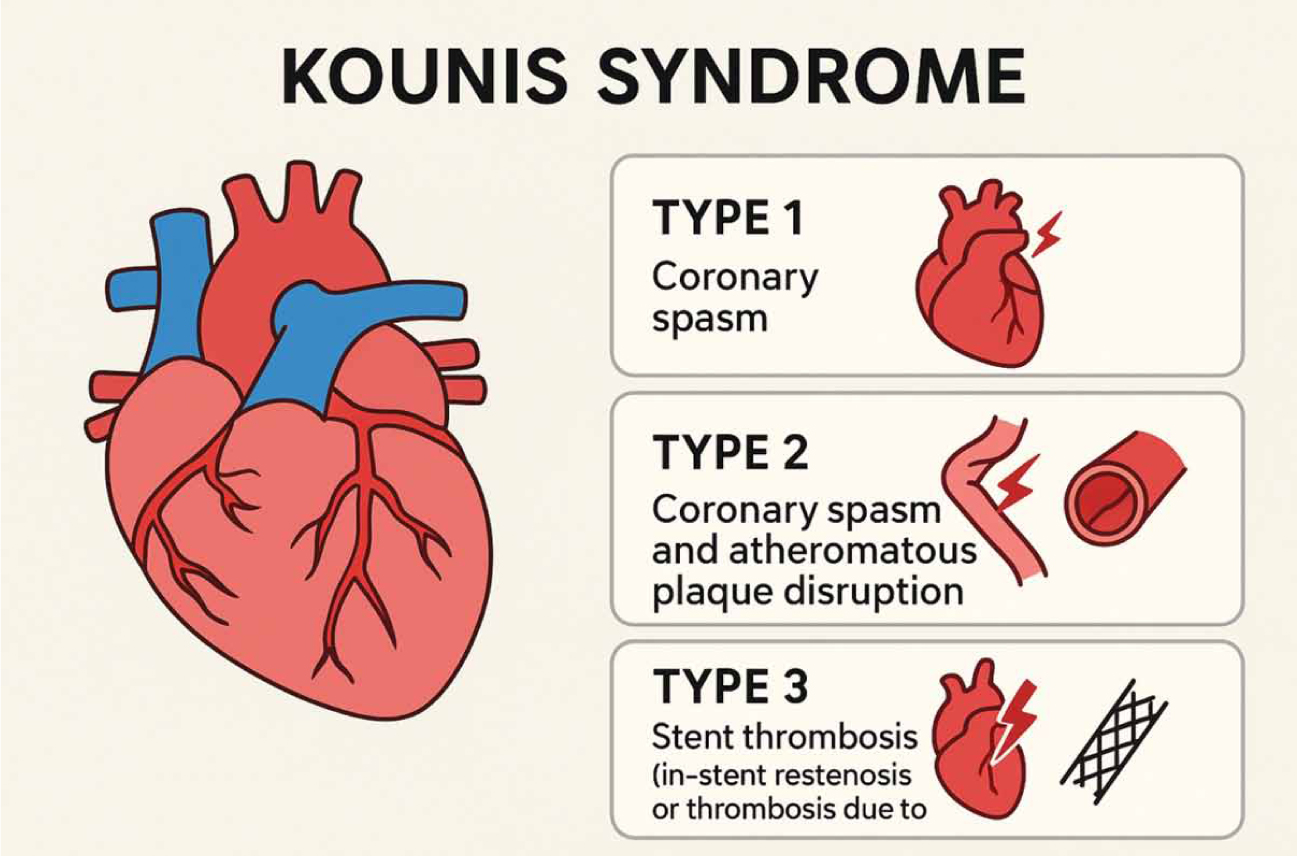
Figure 1. The types of Kounis syndrome associated with coronary arteries.
The majority of the human body’s organs, including the brain, cerebral arteries, and mesenteric arteries, include mast cells. Mast cell activation diseases have also been observed to exhibit signs of cerebral vasospasm, similar to those seen in Kounis syndrome. In another instance, an allergic response to diclofenac caused Kounis-like abdominal pain syndrome in a patient with chronic atherosclerotic mesenteric artery disease. Following anaphylaxis, the patient reported experiencing gastrointestinal bleeding, may have been a consequence of the allergic event [3]. Furthermore, Kounis syndrome is not a vascular disease that affects only one organ; rather, it is a multisystem disorder. Inflammatory mediators that cause this illness are released when mast cells and other related cells, including T lymphocytes, macrophages, and eosinophils, degranulate during an allergic attack, with platelets also participating in this process.
Common Pathway Between Allergic and Non-Allergic Events
There is a common pathway linking allergic and nonallergic coronary events in nonallergic postmortem acute myocardial infarction patients. In comparison to nearby vascular areas or even farther-flung arterial segments, studies have shown a significantly higher (200:1) degree of mast cell degranulation at the sites of atherosclerotic plaque rupture. The issue in these studies was how such high numbers of degranulated mast cells were discovered at plaque rupture or rupture sites given that mast cell maturation and mediator release might take days or weeks. At the rupture site prior to the acute coronary event, mature mast cells that are prepared to degranulate and release their contents are most likely present [4].
Reducing the development of unstable lesions and coronary plaques could have significant therapeutic and clinical implications if mast cell degranulation and the resulting acute myocardial infarction are inhibited. The next generation of therapeutic approaches that can prevent acute coronary and cerebrovascular events may actually include monoclonal antibodies that shield the mast cell surface, as well as drugs and natural compounds that stabilize the mast cell membrane [5].
Mast Cell Degranulation Inhibition may Help Avoid Myocardial Infarction and Thrombosis
Inhibiting mast cell degranulation can help prevent thrombosis and myocardial infarction. It is possible to prevent mast cell activation and degranulation through the following approaches [6]:
- Targeted drugs have limited potential to block stem cell factor (SCF) due to the toxicity associated with mast cell activation. But by adding transmembrane mast cell factor (also called stem cell factor) to lipid nanodiscs or proteoliposomes, mast cell activation can be avoided. These therapies may offer preventive and therapeutic benefits without presenting any hazards.
- Mas-related G protein-coupled receptor X2 (MRGPRX2) is a mast cell receptor that results in IgE-independent degranulation and has been connected to a number of mast cell-mediated diseases. MRGPRX2 antagonists have the ability to prevent mast cell degranulation.
- Humanized monoclonal antibodies, such as omalizumab against IgE antibodies, have already been successfully used to treat recurrent Kounis syndrome in order to treat IgE-mediated coronary syndromes.
- Moreover, dexamethasone has been used to lower inflammation and sodium cromoglycate to stabilize the mast cell membrane, preventing late thrombotic events.
Why Kounis Syndrome Does Not Occur in Every Allergic Reaction
Total blood IgE levels are much greater in individuals with multi-vessel disease than in those with single-vessel disease. They are independent predictors of an increased risk of multi-vessel disease and aid in differentiating the severity of coronary artery disease from traditional cardiovascular risk factors [7]. Numerous investigations have shown that serum IgE levels are higher during acute coronary syndromes [8], underscoring the significance of keeping an eye on these levels in individuals with a history of coronary events. Therefore, elevated IgE levels in cardiovascular disease patients before the coronary event [9] and their association with ischemic heart disease might be a precursor to atherogenesis and its consequences, thereby aiding in the prediction of recurrent coronary events.
Omalizumab (anti-IgE) and mepolizumab (anti-interleukin-5 [IL-5]), two important monoclonal antibodies, are being researched and used in relation to allergic coronary events. The humanized monoclonal anti-IgE antibody omalizumab, which is currently in clinical use, bonds to the constant region (cε3) of the IgE molecule and stops free IgE from interacting with IgE receptors FcεRI and FcεRII, thereby reducing circulating IgE levels. Regardless of how specific an allergen may be, omalizumab can block the responses it triggers because it does not attach to the variable allergen-specific region of the IgE molecule. By not binding to cell-bound IgE, omalizumab prevents the FcεRI cross-linking that may cause allergy, hypersensitivity, or anaphylaxis [10] (Figure 2).
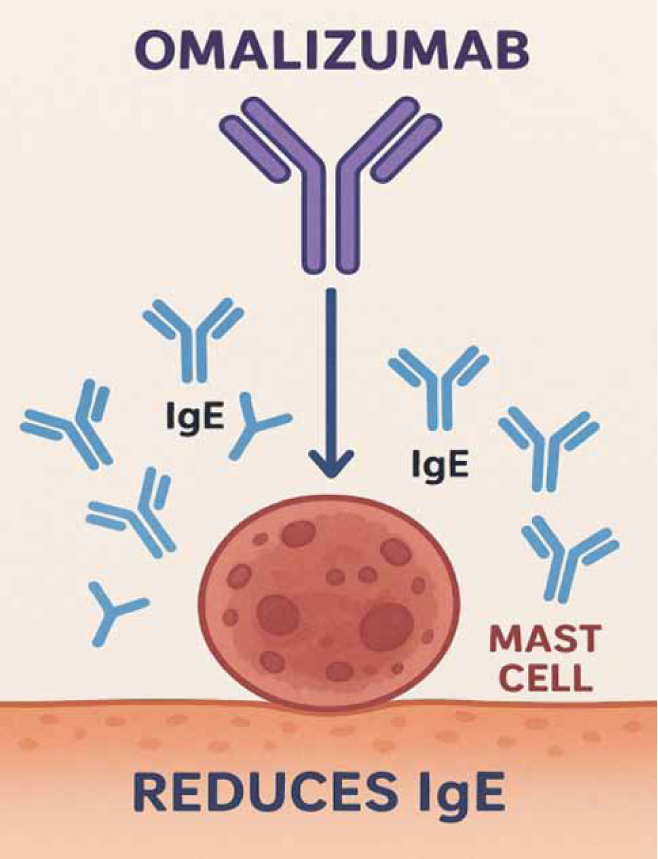
Figure 2. Reducing IgEs can help people who are susceptible to allergic angina and myocardial infarction.
Therefore, reducing IgEs can protect those who are susceptible to allergic angina and allergic myocardial infarction [11]. Furthermore, the reason why not every patient who has an allergic reaction also has Kounis syndrome seems to be addressed by the following: because their blood’s IgE levels are lower.
Conflict of interest disclosure
None to declare
Declaration of funding sources
None to declare
References
- Kounis NG, Koniari I, Velissaris D, Tzanis G, Hahalis G. Kounis Syndrome—not a Single-organ Arterial Disorder but a Multisystem and Multidisciplinary Disease. Balkan Med J. 2019;36(4):212-21.
- González-de-Olano D, Alvarez-Twose I, Matito A, Sánchez-Muñoz L, Kounis NG, Escribano L. Mast cell activation disorders presenting with cerebral vasospasm-related symptoms: a “Kounis-like” syndrome? Int J Cardiol. 2011; 150(2): 210-1.
- Goto M, Matsuzaki M, Fuchinoue A, Urabe N, Kawagoe N, Takemoto I, et al. Chronic atherosclerotic mesenteric ischemia that started to develop symptoms just after anaphylaxis. Case Rep Gastroenterol. 2012; 6(2): 300-8.
- Kounis NG, Stefanidis A, Hun MY, Ozkan U, de Gregorio C, Ceasovschih A, et al. From Acute Carditis, Rheumatic Carditis, and Morphologic Cardiac Reactions to Allergic Angina, Allergic Myocardial Infarction, and Kounis Syndrome: A Multidisciplinary and Multisystem Disease. J Cardiovasc Dev Dis. 2025; 12(9):325.
- Worrall WPM, Reber LL. Current and future therapeutics targeting mast cells in disease. Pharmacol Ther. 2025; 273: 108892.
- Kounis NG, Mplani V, Koniari I. Kounis syndrome: A natural paradigm for preventing mast cell activation-degranulation. Int J Cardiol. 2025;419:132704.
- Kounis NG, Hahalis G. Serum IgE levels in coronary artery disease. Atherosclerosis. 2016; 251:498-500
- Kounis NG, Mazarakis A, Almpanis G, Gkouias K, Kounis NG. Tsigkas G. The more allergens an atopic patient is exposed to, the easier and quicker anaphylactic shock and Kounis syndrome appear: Clinical and therapeutic paradoxes. J Nat Sci Biol Med. 2014: 5(2):240–4.
- Zhang L, Zhu Y, Meng X, Zhang Y, Ren Q, Huang D, et al. Smoking, immunity, and cardiovascular prognosis: a study of plasma IgE concentration in patients with acute myocardial infarction. Front Cardiovasc Med. 2023;10:1174081.
- Kounis NG, Koniari I, Tsigkas G, Davlouros P. Humanized Monoclonal Antibodies Against IgE Antibodies as Therapy for IgE-Mediated Coronary Syndromes: Are We There Yet? Can J Cardiol. 2020;36(6):816-9.
- Forzese E, Pitrone C, Cianci V, Sapienza D, Ieni A, Tornese L, et al. An Insight into Kounis Syndrome: Bridging Clinical Knowledge with Forensic Perspectives. Life (Basel). 2024 ;14(1):91.